The SBU (Swedish Council on Health Technology Assessment) is charged by the Swedish government with assessing health care treatments. Their recent acceptance of low-carbohydrate diets as best for weight loss is one of the signs of big changes in nutrition policy. I am happy to reveal the next bombshell, this time from the American Diabetes Association (ADA) which will finally recognize the importance of reducing carbohydrate as the primary therapy in type 2 diabetes and as an adjunct in type 1. Long holding to a very reactionary policy — while there were many disclaimers, the ADA has previously held 45 – 60 % carbohydrate as some kind of standard — the agency has been making slow progress. A member of the writing committee who wishes to remain anonymous has given me a copy of the 2014 nutritional guidelines due to be released next year, an excerpt from which, I reproduce below.
Nutrition Therapy Recommendations for the Management of Adults With Diabetes
This position statement on nutrition therapy for individuals living with diabetes replaces previous position statements, the last of which was published in 2013 [1] and incorporated into the Standards of Medical Care of 2014 [2]. In particular, evidence suggests that the starting point for therapy for type 2 diabetes and adjunct treatment of type 1, should be some form of very low-carbohydrate diet. The amount of carbohydrates is the most important factor influencing glycemic response after eating and should be considered when developing the eating plan. Carbohydrate intake has a direct effect on postprandial glucose levels in people with diabetes and is the primary macronutrient of concern in glycemic management. While it is still recognized that there is not an ideal percentage of calories from carbohydrate for all people with diabetes, carbohydrate intake should be as low as possible for most people.
There are several good references for implementation [3, 4] although the degree of reduction of dietary carbohydrate should be based on individualized assessment of current eating patterns, preferences, and metabolic goals. Collaborative goals should be developed with the individual with diabetes. For good health, any carbohydrate intake should come from vegetables, fruits, legumes, and dairy products rather than intake from other carbohydrate sources, especially those that contain high starch and sugar. In recognizing the importance of removing carbohydrates, the current guidelines deviate from, and consider inappropriate, previous recommendations from 2008 [5] that “sucrose-containing foods can be substituted for other carbohydrates in the meal plan or, if added to the meal plan, covered with insulin or other glucose lowering medications.” While substituting sucrose-containing foods for isocaloric amounts of other carbohydrates may have similar blood glucose effects, it is now recommended that consumption should be minimized to avoid displacing nutrient-dense food choices.
Recommendations for low-carbohydrate diets.
The new recommendations emphasizing low-carbohydrate diets follow from the observations noted previously [5] that improvements in serum lipid/lipoprotein measures including improved triglycerides, VLDL triglyceride, and VLDL cholesterol, total cholesterol, and HDL cholesterol levels are now recognized as a reliable feature of lower-carbohydrate diet compared with higher carbohydrate intake levels. Through the collaborative development of individualized nutrition interventions and ongoing support of behavior changes, patients should understand the rationale of carbohydrate restriction and be made aware of its potential value.
Most important for clinicians is understanding results of two independent comparative studies from the laboratories of David Jenkins [6] and of Eric Westman [7] shown in Figure 1.
 Figure 1. Comparison of High Cereal and Low Glycemic Index Diets and of Low Glycemic Index Diets and Low Carbohydrate Diets
Figure 1. Comparison of High Cereal and Low Glycemic Index Diets and of Low Glycemic Index Diets and Low Carbohydrate Diets
The role of body mass in diabetes.
More than three out of every four adults with diabetes are at least overweight, and nearly half of individuals with diabetes are obese. Because of the relationship between body weight (i.e., adiposity) and insulin resistance, weight loss has long been a recommended strategy for overweight or obese adults with diabetes. Two important experimental results bear on the new recommendations. First, in numerous trials, low-carbohydrate diets of one type or another out-perform other diets to which they are compared. No diet is better than carbohydrate restriction for weight loss. However, it has been shown that the features of both type 1 and type 2 diabetes are improved by low-carbohydrate diets even in the absence of weight loss.
Previous recommendations on nutritional therapy have failed to take account important work of Nuttall and Gannon who have clearly shown that the symptoms of type 2 diabetes can be improved without the requirement for weight loss [8-10]. Even under weight-maintenance conditions, dietary carbohydrate restriction dramatically improves glycemic control as well as HbA1c and lipid markers. This fact is important given the resistance that many individuals show to weight loss. A series of papers from Nuttal and Gannon [8-10] measured many hormones and parameters in response to various carbohydrate-reduced diets. Although the percentage of carbohydrate differed in many of these studies, the most effective level of carbohydrate in improving the markers was the lowest level of carbohydrate used. Results from one study from Nuttall and Gannon’s lab [10] are shown in Figure 2. A low-carbohydrate (20% energy) diet was instituted for five weeks under conditions where weight was maintained. It is clear from the figure 24-hr integrated and postprandial glucose as well as hemoglobin A1c was improved after the five-week diet period (●) compared to performance before (▲). These results contrast with outcomes from low-fat and calorie-restricted diets, which generally require weight loss for diabetes symptoms to improve. While the results have recently been extended to longer periods [8], it is important to recognize that nothing in the results contradicts the idea that benefit will continue to accrue as long as the diet is adhered to.
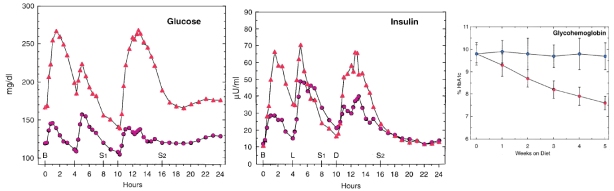 Figure 2. Comparison of blood glucose, endogenous insulin and glycosylated hemoglobin in sixmales with mild untreated type 2 diabetes fed a low-carbohydrate/ high-protein diet (non-ketogenic;20% carbohydrate, 30% protein). Results are shown before (▲) and after (●) the five-week regimen.
Figure 2. Comparison of blood glucose, endogenous insulin and glycosylated hemoglobin in sixmales with mild untreated type 2 diabetes fed a low-carbohydrate/ high-protein diet (non-ketogenic;20% carbohydrate, 30% protein). Results are shown before (▲) and after (●) the five-week regimen.
It is now recognized that the amount of dietary saturated fat and cholesterol recommended for people with diabetes is the same as that recommended for the general population. Recent studies have confirmed that there is no relation between dietary saturated fat and cholesterol and cardiovascular disease [11-13]. Previous statements that “patients on low-carbohydrate diets, monitor lipid profiles” is no longer considered appropriate although all patients with diabetes should monitor their lipids.
Is this real? Can you believe it?
Is this real? No. It’s not real. It could be real if the American Diabetes Association adopts it. You believed that it was real because it is reasonable and it follows from both common sense and scientific principles. You believed it because it provided you with the data rather than giving you the opinion of a committee that chose whatever studies it wanted to, and took the conclusions at face value. Most of all, you believed it because we all want to believe it. Previous guidelines from the ADA have been incomprehensible and ultimately embarrassing. Since the principles of low-carbohydrate diets are so reasonable, bloggers and others have continually tried to find signs of their acceptance in each new position statement from the ADA, signs that could be described as “encouraging first steps.” Invariably, the ADA guidelines have been, instead, the camel-like creations of a committee characterized by stultifying clichés — one reason that you might have believed that the version above was real is that I included trivial phrases — the text that is in blue — from the 2013 guidelines. I wrote this because several bloggers tried to put a positive spin on the 2013 guidelines and I was going to comment on how little it would have taken for them to get it right. So I decided to write it for them.
Imperial Dishabilement. Critique of the 2013 Guidelines
Diabetes Care is the house organ of the ADA. The 2013 guidelines are subject only to internal review. No real peer review is possible and it shows. We are not supposed to be too critical, however. Standards of propriety are expected of the reader. We are supposed to refrain from blunt criticism of style and content, like Robert French’s critique of A companion to Woody Allen in the Times Literary Supplement (October 4, 2013):
“The book is 90% of obfuscation, 10% illumination. Statements of the obvious abound (‘Like many Christians, Jews, Muslims and others, Allen can practice a faith without always believing in it’).”
We are expected to ignore fatuous remarks stating that one of the goals of nutrition therapy is:
“To maintain the pleasure of eating by providing positive messages about food choices while limiting food choices only when indicated by scientific evidence.”
I admit that I had to ask an English professor for an explanation as to why this particular line is so annoying. “It implies that there is some agency out there who wants to deny you pleasure or unjustly limit your food choices.” But statements of the obvious do abound. Some examples:
“For overweight or obese adults with type 2 diabetes, reducing energy intake while maintaining a healthful eating pattern is recommended to promote weight loss.” (twice)
“Personal preferences (e.g., tradition, culture, religion, health beliefs and goals, economics) and metabolic goals should be considered when recommending one eating pattern over another.”
“A healthful eating pattern, regular physical activity, and often pharmacotherapy are key components of diabetes management.”
“Effective nutrition therapy interventions may be a component of a comprehensive group diabetes education program or an individualized session achieved.”
“Health professionals should collaborate with individuals with diabetes to integrate lifestyle strategies that prevent weight gain or promote modest, realistic weight loss.”
All such documents have a certain degree of boiler plate but here it is relentless and overpowering and it takes the place of the science. And it protests too much. “Individualized” appears 21 times in the guidelines. But it is disingenuous. Individualized is just what the previous guidelines were not and those recommendations are specifically not retracted. It is not sufficient to say that your paper “replaces previous position statements.” You have to explain what the previous ones were and why they are no longer applicable.
If therapy is individualized, what principles is individualization based on? “Individuals who have diabetes should receive individualized Medical Nutrition Therapy (MNT) as needed to achieve treatment goals, preferably provided by a registered dietitian (RD) familiar with the components of diabetes MNT.” In other words, you’re on your own, or worse, turn it over to the RD’s. Where do the RD’s get their understanding of diabetes MNT? Well, probably from the last implementation of the ADA guidelines which were unabashed in what they opposed:
“Low-carbohydrate diets might seem to be a logical approach to lowering postprandial glucose. However, foods that contain carbohydrate are important sources of energy, fiber, vitamins, and minerals and are important in dietary palatability” [5] and…
“For weight loss, either low-carbohydrate or low-fat calorie-restricted diets may be effective in the short term (up to1 year).”
But:
“For patients on low-carbohydrate diets, monitor lipid profiles, renal function,and protein intake (in those with nephropathy), and adjust hypoglycemic therapy as needed.”
In other words, low-carb diets are okay if you don’t mind having a heart attack or kidney failure (oh, of course only if you have nephropathy; it’s not a failure to understand of English usage that puts the disclaimer in the wrong place in the sentence ) and the low-carb diet will lead to hypoglycemic episodes.
Most of all, you have to provide new guidance. But guidance is not available in the 2013 position statement. :
“The optimal macronutrient intake to support reduction in excess body weight has not been established.”
“Evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein, and fat for all people with diabetes; therefore, macronutrient distribution should be based on individualized assessment of current eating patterns, preferences, and metabolic goals.”
“The evidence suggests that several different macronutrient distributions/eating patterns may lead to improvements in glycemic and/or CVD risk factors (88). There is no “ideal” conclusive eating pattern that is expected to benefit all individuals with diabetes (88). ” (Reference 88 is to the same group’s review of low carbohydrate diets).
Evidence does not generally suggest what is not ideal. This is especially true if you don’t look at all the evidence and this is the ADA guideline’s greatest failing. The two figures above, by themselves, constitute a strong case for low carbohydrate diets. These papers are not cited by the 2013 guidelines although I have personally pointed them out to members of the committee. Non-scientists ask me: “Can you do that? Can you just leave out relevant papers?”
And “ideal” may not be possible anywhere in medicine. What you want is best practice or, as we describe it, the “default diet,” what you try first, your best bet.
The bottom line is that the 2013 guidelines are weak on science and dreadful in style. The two are closely linked. Obfuscation rather than clarification. The emperor is naked. The document would never survive real peer review. In the end, we have to ask why this is tolerated. The answer is usually that the ADA is a private organization and they may do as they choose. Or are they? They are tax exempt and their officers and editors have federal grants. On publication, Diabetes Care is their journal and the editors can publish whatever they like. Or can they? Is any paper in such a publication to be believed if there is this level of bias among the editors? Are they accountable at all?
The writing committee.
There are no real credentials in science. We all accept that a major part of our understanding of the physical world comes from a clerk in a patent office. But that’s only true if the science is correct. So who did the ADA get to present their position? The list is below. You can Google them to see their qualifications. There are two PhD’s and, oddly, only one representative of the M in MNT (Medical Nutrition Therapy), Will Yancy, who, in fact, has provided strong evidence supporting low-carbohydrate diets. Yancy is a co-author on the un-cited study in Figure 1 (ref. 4). The first author of the 2013 Guidelines, Allison Evert has two publications: those Guidelines and the review paper on low-carbohydrate diets, a subject with which she appears to have no experience. Most of the other authors also appear to have no experience with research on the effects of macronutrients. Most have little research experience at all. As for Yancy, who has made a major contribution to dietary carbohydrate restriction, it is generally assumed that they threatened his life.
Allison B. Evert, MS, RD, CDE
Jackie L. Boucher, MS, RD, LD, CDE
Marjorie Cypress, PhD, C-ANP, CDE
Stephanie A. Dunbar, MPH, RD
Marion J. Franz, MS, RD, CDE
Elizabeth J. Mayer-Davis, PHD, RD
Joshua J. Neumiller, PharmD, CDE, CGP, FASCP
Robin Nwankwo, MPH, RD, CDE
Cassandra L Verdi, MPH, RD
Patti Urbanski, MED, RD, LD, CDE
William S. Yancy, Jr., MD, MHSC
Bibliography
1. American Diabetes Association: Nutrition Recommendations and Interventions for Diabetes–2013. Diabetes Care 2013, 36(Suppl 1):S12-S32.
2. Association AD: Standards of Medical Care in Diabetes — 2014. Diabetes Care 2014, 37, Supplement 1:S15-S80.
3. Bernstein RK: Dr. Bernstein’s diabetes solution : the complete guide to achieving normal blood sugars, 4th edn. New York: Little, Brown and Co.; 2011.
4. Vernon MC, Eberstein JA: Atkins Diabetes Revolution. The Groundbreaking Approach to Preventing and Controlling Type 2 Diabetes. New York: William Morrow; 2004.
5. American Diabetes Association: Nutrition Recommendations and Interventions for Diabetes–2008. Diabetes Care 2008, 31(Suppl 1):S61-S78.
6. Jenkins DJ, Kendall CW, McKeown-Eyssen G, Josse RG, Silverberg J, Booth GL, Vidgen E, Josse AR, Nguyen TH, Corrigan S et al: Effect of a low-glycemic index or a high-cereal fiber diet on type 2 diabetes: a randomized trial. JAMA 2008, 300(23):2742-2753.
7. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR: The Effect of a Low-Carbohydrate, Ketogenic Diet Versus a Low-Glycemic Index Diet on Glycemic Control in Type 2 Diabetes Mellitus. Nutr Metab (Lond) 2008, 5(36).
8. Gannon MC, Hoover H, Nuttall FQ: Further decrease in glycated hemoglobin following ingestion of a LoBAG30 diet for 10 weeks compared to 5 weeks in people with untreated type 2 diabetes. Nutr Metab (Lond) 2010, 7:64.
9. Gannon MC, Nuttall FQ: Control of blood glucose in type 2 diabetes without weight loss by modification of diet composition. Nutr Metab (Lond) 2006, 3:16.
10. Gannon MC, Nuttall FQ: Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes 2004, 53(9):2375-2382.
11. Forsythe CE, Phinney SD, Feinman RD, Volk BM, Freidenreich D, Quann E, Ballard K, Puglisi MJ, Maresh CM, Kraemer WJ et al: Limited effect of dietary saturated fat on plasma saturated fat in the context of a low carbohydrate diet. Lipids 2010, 45(10):947-962.
12. Jakobsen MU, Overvad K, Dyerberg J, Schroll M, Heitmann BL: Dietary fat and risk of coronary heart disease: possible effect modification by gender and age. Am J Epidemiol 2004, 160(2):141-149.
13. Siri-Tarino PW, Sun Q, Hu FB, Krauss RM: Saturated fat, carbohydrate, and cardiovascular disease. Am J Clin Nutr 2010, 91(3):502-509.
My 14 year old son has type 1 and is on a low carb diet. His blood work is absolutely perfect!
It seems like such diet should be the first thing offered. Is this what happened?
Meanwhile, . . . a tidbit in a magazine I picked up this afternoon, stated that X-number of millions now have Type 2 diabetes. It then presented 3 or 4 bizarre things and the reader was to guess which substance was being considered for a new wonder drug for the treatment of Type 2 diabetes.
What were they? And which one was the new wonder drug?
I’m sorry. I didn’t pay a lot of attention. I think the magazine was “National Geographic,” though that seems a bit incongruous. I didn’t bother to check out the “right answer.” The whole thing seemed stupid and I just turned to the next page. My thought at the time was “every way but the right way.”
Awesome, I believed it and thought a miracle had at long last happened. Very well written! I almost sent an email to Dr. Bernstein telling him that his book (and Atkins Diabetes Revolution) were both now recommended!
The theme song of Nutrition & Metabolism Society is the Billie Holiday song that has the line: “the difficult we do right now. The impossible will take a little while.”
Me too, almost wept when I realised it was only wishful thinking x
I’m sorry for the let-down but you might write to the ADA and ask what’s standing in their way. Let us know what they say.
That was a cruel post, Richard. I admit being total drawn in…it felt so wonderful as I was reading it. Thanks for a preview of what might be reality a decade or 2 down the road (I’m an optimist). My doctor and I agree to disagree on the wisdom of low carb. He warned me that it might be 10 or more years before the benefits of low carb are embraced by mainstream. He is probably correct on that, but doesn’t change the truth. Courage for now, vindication for later.
It won’t take ten years. Dreadful as the 2013 guidelines are they are a sign that they slouching toward low carb. Again, as noted above, you can look into the future at :http://wp.me/p16vK0-2
I was so hoping this was true, for the sake of millions of diabetics who trust their doctors too much and their own capacity for understanding research on the subject, too little.
The sad part is that when they finally realize that they trusted their doctor too much, they will be inclined to distrust them on things that they are really well trained for, like the practice of medicine.
Wow! You really had me going there. I was ready to send
this link on to everybody I know.
So sorry it’s not real. Maybe next year…or the next… or…
You can send it to everyone you know because they may be more important than the ADA. At some point the ADA will be superfluous altogether.
Why Not? Most of the people that I know have diabetes, over weight, some obese ! They are eating foods that are high in Carbs. I know people that when they eat a lot of carbs… They are admitted to a hospital, to try and clean things up…Their body can’t handle it….
You can ask the authors of the guidelines or others at the ADA why not. There are a couple of YouTubes where I have challenged them but I didn’t get very good answers maybe you’ll do better.
Looking into the future it may be faster than you think:http://wp.me/p16vK0-2Y
I thought it was too good to be true. At least the recent ADA dietary guidelines released last month did finally acknowledge that the macronutrient mix is a one size doesn’t fit all situation. Namely they acknowledge that for some individuals, a low carbohydrate diet is best and on page 7 they state that there is evidence that low carbohydrate, high fat diets likely have lipid profile benefits
Click to access dc13-2042.full.pdf
Actually, they’ve admitted this for years. The 2008 guidelines say “Changes in serum triglyceride and HDL cholesterol were more favorable with the low carbohydrate diets. In one study, those subjects with type 2 diabetes demonstrated a greater decrease in A1C with a low-carbohydrate diet than with a lowfat
diet (20). A recent meta-analysis showed that at 6 months, low carbohydrate diets were associated with greater improvements in triglyceride and HDL cholesterol concentrations than low-fat diets; however, LDL cholesterol was significantly higher on the low-carbohydrate diets (21). Further research is needed to determine the long-term efficacy and safety of low-carbohydrate diets (13).”
Get it? The low-carbohydrate diet is better than the low-fat diet in the short term so it is the long term effect of the better diet that we’re worried about.
Right. They still can’t get over the Ansel Keys brain washing that fats are the cause of heart disease not carbohydrates and metabolic syndrome. Still focusing on LDL despite the fact that the elevated LDL associated with low carb diets has been converted from small dense pattern B to large buoyant harmless pattern A type associated with reversal of metabolic syndrome.
GREAT news!! Only about 50 years of lies and junk science…
rdfeinman posted: “The Swedish Health Ministry’s acceptance of low-carbohydrate diets as best for weight loss is one of the signs of big changes in nutrition policy. I am happy to reveal the next bombshell, this time from the American Diabetes Association (ADA) which will “
Has it been that long?
Congratulations, Richard. I know you’ve been working hard on this for many years. Great news!
Pete Farnham
Thanks, Pete, but you may want to read the whole post.
Knew it was too good to be real. A type 1 diabetic since 1970, I have come to hate the ADA with a hatred that shocks even me. They even provide food-exchange figures for packages of Pop-Tarts, the whores. I’m not sure that my retinopathy, impotence, neuropathy, etc. would have been less severe without twenty years of pasta and tortillas and wheat cereals with skim milk, but I suspect that I was robbed of health as well as delicious food for much of my life. It’s hard to forgive them.
Many of us are surprised at the level of hostility that they have been able to generate.
There isn’t anyone out there who wants to put there neck on the line…Look around yourself. Your families, friends. How many of them are diabetics? I am from a family of five, four of these are diabetics. They are on insulin everyday. There eating habits are different than mind, all high carbohydrates eaters. I’m 63 years and don’t eat as much, I walk, exercise, and try and eat the right foods. Loose weight, get out of the house from that lazyby, get with the proramme.. in short.. there are so many people that can and would become healthy, They say, ” You are what you eat”. Fat, obese, with high blood pressure, and a diabetic.. Its time for the people to stand up to the ADA, get better results for everyone, Give information , straight and to the point. in place of collecting big pay checks…Most doctors only know what they are forced feed…. Its your life that they are playing with.. Someone out there should have better answers?
The movement rests with the people. If we don’t tolerate the stuff from the ADA, they will change. Write to them. Polite and concise. Ask. Don’t tell. Tell them that you will post the answers on Facebook — at least post your question and others will follow you
Richard, and even if it would eventually become a healthy low carb, what type of fat do you expect they will recommend to get the energy from? PUFA’s ? So the diabetic can replace diabetes with an increase risk of developing a neurodegenerative disease,because Omega 6 will screw up the pathways with too much ROS and too much RNS
Possible duplicated message (may have hit wrong button).
We don’t want them to recommend anything. We want neutral body, National Science Foundation, or similar to get all the facts from us and from them. A neutral analysis of the data will tell us what can be recommended.
And this is where I get really pessimistic ” a neutral analysis of the data”. Do you realize what you are asking here? Just finished reading A Lifelong Fight Against Trans Fats
Dr Fred Kummerow 99 years old, in a wheel chair. His wife of 70 years died of Parkinson’s died last year at the age of 94. His lifelong healthy diet has been whole milk and whole grain. (beside veggies and fruit and meat. Ask David Perlmutter about that kind of diet. I don’t like the wheel chair and I like Parkinson’s even less.
Ron Rosedale may going a little overboard on there are no safe starches, I am willing to take that gamble a long way. Maybe add some resistant starch onoccasion to keep my colon cells supplied with healthy butyrate food.
I agree that I may be suggesting the impossible but we certainly have a crisis in nutrition. I don’t even know if trans-fat is as beg a problem as they want to say it is.
[…] Dr Feinman uttrycker sitt missnöje på sin blogg där han först skriver hur riktlinjerna skulle kunna sett ut, ganska roligt faktiskt: ”American diabetes association embraces low-carbohydrate diets” […]
[…] The Swedish Health Ministry’s acceptance of low-carbohydrate diets as best for weight loss is one of the signs of big changes in nutrition policy. I am happy to reveal the next bombshell, this tim… […]
damn, I thought it was real! Even if it were real, for the change to propagate to all levels throughout the entire world would have probably taken more than 10 years, the least to say…as many doctors would be skeptical to adopt a vlcd.
I am not so sure. The ADA Nutrition Committee does not speak for the rank and file. Many physicians and diabetes educators know the value of carbohydrate restriction — how could they not? And most physicians have their patients as the first priority. Very few of them have the time or inclination to fight with the ADA. And, in fact, the key word is cognitive dissonance. In some way, the ADA knows that they must switch. The current guidelines are slightly more flexible as they try to back into best treatments while saving face and avoiding law suits, what I call slouching towards low-carb. But if your child had type2 diabetes and you found out that they could have offered better treatment while, instead, they sought the most politically expedient strategy, you might be angry.
Well doc, I’ve heard that’s also difficult for them to prescribe treatments contrary to the general guidelines. So, when doctors have patients with diabetes, they somehow need to follow the guidelines right? Well, that sucks.
And we also know that some of the physicians try low-carb diets themselves, so they know it works. Does it mean that they hands are tied? Who is gonna push the change? I really wonder…
Will the change come from the people? Can you think of this scenario?
No. It would be not difficult at all if they know how. Real (modified) conversation:
RDF: Do you recommend a low-carb diet?
MD: I may recommend it but I don’t have the resources to follow up.
RDF: What do you do?
MD: I send them to a dietitian.
RDF: Can you send them to a dietitian who will help them with low-carb?
MD: I don’t know any dietitians who will do low-carb.
Now, a dietitian could get in trouble for doing low-carb but many do it anyway.
Of course, in some specific areas, like epilepsy, they cannot get reimbursed from insurance company.
Physicians who go on low-carb diets themselves may have the sense that they are experimenting — the los fat idea was sold big –and don’t want to do that on their patients.
The fault is with the ADA, AHA and USDA panels who, whatever their motivations, are keeping America fat and diabetic. But they are far from invulnerable. So…
YES. The change must come from the people. What we want is a truly impartial panel of real scientists from other fields — i.e., trained in scientific method but without a horse in the race (no nutritionists) who can hear testimony from everybody including me. Probably the government is the only body who could do it, via NIH, NSF or other agencies. The people can ask for that. It could even be done at a state or local level.
But the people can start now. If you write to the authors of the ADA guidelines and ask why they won’t do right. Be polite. Be concise although you can anticipate arguments in advance — low carb has better compliance than other diets, diabetes is disease of carbohydrate intolerance so burden of proof on anybody who says anything else, etc. Be polite. Ask. Don’t tell. Also, you can collect the testimony of people like some of those who have made comments here. Only crowd-sourcing will stop them. Encourage others to go to government and private agencies and the press. Collect the answers from these agencies. There is tremendous power of the consumer now. Maybe start writing reviews of the ADA. If you get everybody moving, it will change overnight. You can write about it. People will read it and you will get rich.
Is that a good scenario?
[…] I sin blogg har Richard Feinman skrivit sin vision om ADA:s (American Diabetes Association) nya kostråd för 2014. […]
Glad I read the whole thing before commenting. Great article, but it makes me so angry. I’m so glad my son’s doctor isn’t telling him to use the ADA guidelines. He’s T1 and doing great on LCHF.
You can write to them. If you are polite and concise, they will answer you. Ask them how they can ignore what you see as the data. Individualized doesn’t mean anything in recommendations. Individualize is what you do before you talk to an expert. Ask why your doctor knows what works and why isn’t that recommended? If they get enough input, they will have to change. Unfortunately it is up to the people.
http://josefboberg.files.wordpress.com/2013/04/carbs-are-toxic.pdf = about the relationship between the nature diet and better and better health.
Exaggeration will not help us and inaccuracies will be worse. Carbohydrates are not toxic. For many people, there are conditions where high intake will have a toxic effect or, more precisely, reducing carbohydrates are therapeutic — different than saying they cause anything. The metabolism of fructose resembles, in no way, the metabolism of alcohol (beyond the fact that all metabolism is connected). To say that fructose is metabolically like alcohol is to leave all of us open to the charge of ignorant amateurs. Can’t do anybody any good.
[…] American Diabetes Association Embraces Low-Carbohydrate Diets. | Richard David Feinman. […]
Hi Richard. Don’t want to spoil your day, but I’m sending you the post below from a guy on Linked-In. He is really obnoxious and he attacks everything I post. He’s the Nutrition research specialist at Pritikin Longevity Center. I am tired of responding to him and thinking of just leaving the group, but thought I’d see if you would like to weigh in on his rant before I go. I can post a response from you if you don’t want to join the group. It is “Evidence Based Nutrition.”
Hope you are getting a good response to the article–I posted it to all my social media groups.
Judy BB
“At the risk of spoiling the ending this article is just another silly rant from Richard Feinman, in which he pretends the American Diabetes Association now shares his delusional ideology about the health benefits of diet loaded with fatty animal products is optimal for those with diabetes. In the end he admits he’s just making this stuff up and using his pseudoscientific approach to the scientific evidence. All studies that have properly controlled for energy intake have shown that diets higher in saturated fat, cholesterol, and salt elevate numerous CVD risk factors. Since people with type 2 DM are at nearly triple the risk of dying from CVD events as the general population advocating one high in saturated fat and cholesterol as Feinman does makes no sense to the ADA, AHA, and all other credible organizations who have set up expert panels to review ALL the evidence and not just the cherry picked data from poorly designed and interpreted studies. In fact diets higher in saturated fat and cholesterol-rich foods like red meat, egg yolks, cheese, and butter and lower in whole grains, fruits, and vegetables have repeatedly been shown to elevate total-c and LDL-C levels, which means they promote atherosclerosis and lead to heart attacks. This is particularly poor advice for those with type 2 DM, who are at much higher than average risk. ”
By James Kenney, PhD, RD
I might join the group but why should you leave the group? It is important to hear the other side, especially in such a well-argued, well-documented message. The Pritikin diet is one of the choices, just not the first choice for people with diabetes. I once suggested to the spokesperson from the ADA that they were strong on what they didn’t like but not so good on what they do like. She gave me permission to quote her response that that was a fair criticism. Maybe Kenney is like that too.
SBU in Sweden compared the different diets each other the benefit of the Low Carb. It is an independent organisation to assessing health care interventions like Cochrane and not official government office. I m sorry but low carb is not the official view of the diet in Sweden.
http://www.sbu.se/en/
Antti Heikkilä MD
Thanks for this information. The SBU describes itself as “an independent national authority, tasked by the government with assessing health care interventions from a broad perspective, covering medical, economic, ethical and social aspects.” I will edit the post. I don’t know who is on the panel and what their scientific credentials are but any such statement is unusual given the hostile attitudes towards low-carbohydrate diets in the past.
Unfortunately, the Swedish low-carb people are over-enthusiastic. SBU has made the following conclusions, which have been known for a long time. It is regrettable that the Swedish news coverage is a real canard.
http://translate.google.com/translate?hl=en&sl=sv&tl=en&prev=_dd&u=http://www.sbu.se/sv/Publicerat/Gul/Mat-vid-fetma-/
I would certainly agree that we are all trying to find something positive in the SBU statement which I don’t think is a canard (which usually means myth) so much as the incredibly weak, even cowardly statements that you usually get from such organizations. It crosses a line that American agencies barely approach of saying a very little bit that is definitely positive about low-carb diets. Despite its weakness scientifically, however, I think it indicates the old guard looking for a way to face facts. I assume it derives in some way from the attack on Annika Dahlqvist and, in that sense, is a turn-around. But, I agree, that we may be over-enthusiastic.
I can’t seem to find any information now, but somewhere I read that before drugs were developed for diabetes, the standard treatment was to tell diabetics not to eat starch and sweets. I wonder if there are any records of how people fared when they complied carefully with that recommendation. My hunch is that most did well.
I don’t know what kind of data there is. There is a question of the relative prevalence of type 1 and type 2 diabetes. Differences were discovered in 1930’s, ten years after the discovery of insulin. A major fear was ketoacidosis. Eric Westman has published a discussion of some treatments before insulin: https://dl.dropboxusercontent.com/u/37202414/Westman_Hist_Diabetes_BiolMed2006.pdf
After the discovery of insulin, diabetes was treated as a hormone deficiency disease (rather than a system disruption disease) and, in some way, still is so the studies of diet may have included insulin. But, the discussion on the issue is no longer serious. The 2013 ADA guidelines are so pathetic and the fact that they are tolerated means that nobody really wants the answer. IMHO
Thank you! That’s exactly what I was looking for, and more. It’s interesting to see how close they were to the low-carb high-fat answer already then. Too bad the idea didn’t catch on before the current official dietary religion became so entrenched.
There is something obvious about how you treat a disease whose most salient symptom is hyperglycemia and glucosuria. And if you haven’t seen it, there is, with usual self-promotion, the forthcoming history of diabetes http://wp.me/p16vK0-2Y.
Hiya, I believe that before insulin was discovered, a zero carb diet was the only diet that kept T1 and 2’s alive, but only for about 18 months or so after the condtion became apparent. Don’t think it was a high fat diet tho. Pretty much as soon as insulin was discovered and available cheaply the diet adivce became one of eat what you like and treat/compensate the effects with insulin.
I think even now in many clinicians mind, diabetes is perceived as a hormone deficiency disease rather than a systems problem, that is, disruption in metabolism.
“I think even now in many clinicians mind, diabetes is perceived as a hormone deficiency disease rather than a systems problem, that is, disruption in metabolism.”
I think type 1 is, indeed, perceived as a hormone deficiency disease, and it is.
Type 2 is perceived as an insulin resistance disease, even though recent research suggests it’s a relative hormone deficiency disease, that is, enough insulin is produced to cover carbs if you don’t have insulin resistance, but not enough with the IR caused by obesity, especially if you’re eating a lot of carbs.
What causes the IR is of course open to debate. If anyone could come up with a definite answer, I think that person could start booking a flight to Stockholm.
Yes. You are right. I did not describe the situation accurately. Certainly, type 1 is a deficiency disease and with the caveats you mention so is type 2. What I really meant to say is that they are treated with a kind of hormone replacement which is reasonable on the face of it but in practice leads to problems as in the comments below to “eat what you like and treat/compensate the effects with insulin” or more subtly to adjust the insulin to fit the response to food, rather than adjust what you eat according to a meter. As in Dr. Bernstein’s rule of small numbers, smaller amounts of carbohydrate will cause smaller excursions. So, diabetes is a hormone deficiency disease but it is best treated to try to make as few replacements is possible. Are we in agreement?
I have a home medical book from about 1910, and the “diabetic diet” outlined in that book is a lot like Atkins induction. They weren’t t even allowed to eat liver, because of the high levels of glycogen it contains. They were allowed “protein bread,” whatever that is. The problem was that even on a LC diet, the mortality rate for people with type 1 diabetes was 100%. They could extend their lives for a few years on a starvation diet, which was able to keep them out of ketoacidosis (not ketosis), but they often died from the starvation rather than the diabetes itself. I have a friend whose father was being starved in a hospital, and he wrote home ecstatically when they let him have an additional ounce of cheese each day. He was one of the first to get insulin.
This means that most “diabetics” who survived were type 2.
After insulin was discovered, most doctors continued to prescribe LC diets to diabetic patients because that was what they were accustomed to, just as today most doctors continue to prescribe low-fat, high-carb diets, because that’s what they were taught in medical school for the past 40 years.
Back in the 1920s, some physicians (esp. HR Guyelin) claimed that when they gave their patients more carbs, they needed less insulin. Unfortunately, these old papers aren’t online, so it’s difficult to know what the evidence was. The “diabetics” might have been early type 2s who could produce enough insulin when insulin resistance was lowered. Others (esp. Himsworth) said that fat caused insulin resistance. And when the dietary fat-cardiovascular theory became prevalent, the professional groups started recommending more and more carbs, because people with diabetes are at high risk for CVD. “How they fared” depends on how you define it.
Most people with diabetes died from cardiovascular disease. But many people without diabetes also die from CVD. One could claim that dying from CVD suggests immunity to cancer. And insulin preparations in early days were crude and patients didn’t have blood glucose meters to monitor their sugar levels, which were undoubtedly bouncing from low to high, even on a LC diet.
James Anderson, who proposed a high-carb, high-fiber diet for diabetes, admitted that blood sugar levels went very high after eating his diet but said there was no evidence that high blood sugar was damaging. Richard Bernstein was told the same thing when he developed complications on the high-carb ADA diet. However, “no evidence” isn’t the same as “isn’t true,” and later the DCCT study and similar ones showed conclusively that high blood sugar *is* associated with complications. Increased insulin resistance may not matter if you’re not eating a lot of carbs. And the dietary fat CVD hypothesis has been shown to be faulty.
Diabetic diets have been yo-yoing between LC and high carb for centuries. I believe that the LC diet is the best we have at the current time. But the history of science suggests that when you have two philosophies that keep fighting to impose their views, it often turns out that both sides were missing something, often because the technology needed to discover some factor wasn’t available.
So I think people with diabetes should start with LC diets (the default diet, as Richard proposes) but scientists should keep doing research to see if there’s some element to this puzzle that they’ve overlooked. In the 1920s they didn’t know about insulin resistance and type 2 diabetes. Maybe there are subsets of type 1 and type 2 (we already know of some like LADA and MODY and Flatbush diabetes) but there might be others that respond differently to diets and skew the data.
Just my 2 cents which turned out more verbose than I’d intended.
Great 2 cents. I think your point is well taken. Diabetes is a system disease and, at least on first principles, there is no reason that there might not be an ideal level of carbohydrate for particular people but, again, the burden of proof is finding such a level and such a person. Low-carb is the default because of the inherent nature of the problem. In science, you don’t start from zero.
Himsworth, who I believe was the first person to recognize the difference between type 1 and type 2, showed that high carb was better than low carb (~1935). These were well done experiments but, I think that patients may have been on insulin — as I mentioned, diabetes began to be viewed as a hormone-deficiency disease and taking insulin as a virtual definition. And,as you say, not good information on quality of insulin. Those studies were never repeated, however.
[…] Embraces Low Carb Diets in 2014!? American Diabetes Association Embraces Low-Carbohydrate Diets. | Richard David Feinman […]
Re Himsworth: One thing he did was to put people on various diets and then do what was essentially a glucose tolerance test. Those on the high-fat diet tested diabetic. But a high-fat diet is a low-carb diet, and we now know that you have to “carb up” for three days before a GTT or you may test diabetic when you’re not. Starving people also test diabetic. So those results don’t prove much except that if you choose a LC diet, it’s good to stick with it 100% and not 70% or whatever.
He also did studies in which he injected insulin and showed how quickly the insulin reduced blood glucose levels. The decrease was the least in the high-fat group, which suggested insulin resistance.
But does insulin resistance matter when you’re not eating much carbohydrate? That’s a question no one has really answered definitively. I suppose it’s nice to know that the next generations will still have interesting problems to solve (if we don’t blow up the world first).
Thank you, Dr. Feinman and Gretchen, for all the information in answer to what I now realize was probably a naive question. But I’m glad I asked! Yes. I read http://wp.me/p16vK0-2Y when it was published.
I stumbled across your blog as a link in another blog – just reading your section on organic chem – will take me time to digest.
I’m a doc (meds ’81), in the past 2 years I have an all consuming interest in nutrition, modifying my practice according to what I self teach, since the official guidelines are clearly not working with my patients. Your post is right on.
Hoping you may be able to shed some light on a metabolic quandary….I am trying to understand the biochemistry, so that I can suggest appropriate lifestyle/diet modifications.
Is there some mechanism by which the following scenario makes biological sense –
A lean and fit paleo style dieter, at ideal weight (BMI 20), without the markers of Met Synd by WHO criteria – ie, they have, for example, high HDL(>2), low TGs (eg 0.5), normal waist, low BP, low hsCRP(<0.5), BUT high normal FBS (6.0) and A1C (6.0%).
I'm not sure if you know the answer, but maybe you can speculate, would such a person fall into the insulin resistant lean group of people, who are at risk for metabolic consequences?
If carbs intake is low (100 gm/d), how is so much hemoglobin getting glycosylated?
Of note – no hemoglobinopathies or reason to suspect prolonged RBC lifespan.
In the above scenario, the measured fasting insulin level is in the low normal range, with a normal insulin response to food ingestion, so I would have thought that implies normal insulin sensitivity. I’m just wondering what I am missing or misinterpreting.
I thank you in advance for time, I have to pursue and understanding of this issue, but cannot get clarification.
This may be answerable by clinicians and I will run it by them. Other readers may also have comments.
I am *not* a clinician, but I have a few suggestions. A lean person with high BG may be LADA (latent autoimmune diabetes of adults), which is essentially type 1 that appears late (I know a woman who was Dx’d on her 60th birthday). It also progresses more slowly than regular type 1. However if they’re producing normal insulin after eating, that argues otherwise. Fasting insulin is “low normal.” Have you measured more than once, and is it decreasing? They might be early LADA still producing insulin. Have you tested the patient for anti-GAD antibodies, which would suggest LADA?
They may also be MODY, which is a monogenic form of diabetes with little insulin resistance, often found in thin patients. Several different MODYs have been discovered, and there are undoubtedly others we don’t know about. Jenny Ruhl has a MODY page with a lot of information http://www.phlaunt.com/diabetes/14047009.php.
Fasting blood sugar depends on how much glucose the liver is making through gluconeogenesis. Insulin is supposed to dampen gluconeogenesis, but that doesn’t happen if the liver is insulin resistant. This person doesn’t sound insulin resistant, but it’s possible (I don’t know how probable) that the person has insulin resistance in liver but not in muscle.
Finally, some people have slightly higher fasting BG levels on a low-carb diet. But overall BG levels are lower, and the patient’s A1c isn’t consistent with that.
As a patient, I commend you for thinking outside the ADA box and trying to figure out this patient’s physiology.
Hey, thank you for your interest, here is some additional information..
No LADA (C-peptide is normal) or MODY (age 56 and no criteria for diabetes). I figure morning fasting glucagon is high (in the face of low insulin), explaining the high normal FBS from gluconeogenesis.
Physiologic insulin resistance people should have low A1Cs with high FBS. Your classic ketogenic dieter, as you aptly point out.
The local endocrinologists have told me “not to worry – she’s not diabetic” – but I would like to be more proactive.
I appreciate any comments and any help, and thanks Richard for asking around.
I’m not a Doc so can only give you my personal experience. I have a similar profile, VLC diet, high HDL, 3.00 and low triglycerides, 0.68, and also a high HbA1c at 5.9. With a VLC diet glycation level should be much lower, however I suffer from reactive hypoglycemia, not severe but typical functional. My Doc and I suspect this is the cause of the elevated HbA1c. My daughter has a more severe HbA1c condition. This went undiagnosed for 10 years as she went on a downward health spiral resulting from multiple prescription drug side-effects. The fact that the primary cause went undetected by perhaps 20 Docs suggests this is a dietary condition not generally recognized by many Docs. The evidence for this is that following my formal 5 hour test for the condition I copied my data onto a clear multi-color glucose test tolerance chart I found on a medical school website; my Doc asked me to send him a copy of the chart. Eventually Doc 21, a holistic Doc, diagnosed my daughter’s condition in the first five minutes of her first visit, gave dietary advice which began to work immediately then went on to assist in the slow repair of her damaged endocrine system and chaotic and deficient sleep patterns. I wonder what would have eventually happened to her if I had not given her the contact info for the holistic Doc. She is now fully functional once more after losing ten years of her life to a simple condition easily treated by diet. Please do continue to expand your practice of dietary medicine and take every opportunity to speak in detail about it with your colleagues.
@David
So I’m trying to understand what you did for testing – ? a standard 75 gm OGTT but modified it by taking hourly BS readings for 5 hours? You must have done this at home – with a glucometer, since no such test exists in conventional medicine. So your daughter has hypoglycemia too? My patients with hypo never get high enough sugars to be called hyperglycemic, and their A1Cs are normal. I take it the solution for you and your daughter was to eat a high protein/fat diet, with small meals throughout the day? You mentioned you do a VLC diet, are you in the keto range? If so, you shouldn’t need the standard 6 small meals per day.
The person I am describing does not have hypo, in fact, this person practices intermittent fasting (16 hours fast, 8 hour eating window -11am to 7pm), with normal insulin levels during the eating window, no hypo symptoms at any time.
Thank you for sharing your experience.
My endo says if she sees an A1c of 5.8, she knows the person is diabetic and will eventually be Dx’d. But that doesn’t mean my endo is right and the endo you consulted is wrong. Lots of gray areas. And sometimes different labs give different A1c results. I once had an A1c of 5.6 at the local hospital and 7.1 from a mail-in test to a Florida hospital that does diabetes research and used HPLC. Joslin always sends blood to two different labs when results of some study involve A1c, and they never agree.
And everything about your patient is consistent to suggest nondiabetic except the A1c.
MODY can be Dx’d in adults if the symptoms are mild.
Keep digging and disseminating your findings. An interesting puzzle.
I will for sure, because I have 3 similar patients (and I’ve only recently started to case find, because in Canada there are new clinical practice guidelines for diagnosing diabetes, and they rely on A1c rather than the traditional criteria), so this has the ability to impact on many future patients too. It is true that one of these people does have some markers for metabolic dysregulation……and therefore an explanation for the results.
I’ll check out the MODY aspect more thoroughly – thanks for the heads up.
Here are a couple of other comments from experts:
From Katharine Morrison:
I think it would be reasonable in this case to do a glucose tolerance test.
This guy is slim, does NOT have insulin resistance or metabolic syndrome but despite other normal parameters has higher fasting bs and hbaic than you would think is at all “reasonable”.
There are other types of disorders that cause diabetes and maybe he is developing one of these. I have seen 3 patients who were not typical of type one or two but who did need insulin quite soon after diagnosis. The two UK ones never got any clarity on diagnosis.(As is entirely what happens a la NHS) One is doing great low carbing on insulin, one eats quite a lot of carbs but only needs a small basal insulin and gets near normal HbA1cs, and US one has a disorder where the insulin is made in the pancreas but can’t get out. (That’s as much as I know but it is genetically based). She does very well on low carbing and insulin.
From Mike Eades:
In my experience, I’ve found many people on long-term low-carb diets are chronically dehydrated. Chronic dehydration can increase the concentration of sugar in the blood. I’ve had low-carb patients who have developed elevated glucose levels drink 16 ounces of water each morning and at least a couple of glasses of water throughout the day. In each case in which I’ve used this strategy, blood sugar has fallen into the normal range within a week.
Try it and see what happens.
From Valerie Berkowitz:
Maybe Dawn phenomenon or liver related blood sugar issue , not insulin…questions are does he eat before bed and what? maybe he should get up at night 3 am and check BG just to monitor
@ rfeinman
Thank you so much for getting these opinions. I will get a BUN and OGTT on these 2 patients.
One of these patients does IF – no calorie intake from 7pm to 11am, I don’t think Dawn phenomenon – normal LFTs too. I would understand the high am BS as physiologic insulin resistance, but the A1C should be normal as with other low carbers. I’ll keep on plugging away, will let you know if I find anything.
[…] but all this does begin to grate after a bit. (Along the same lines Richard Feyman sports that the ADA is finally recommending low-carb diets. Oh, brother! How long does it take for people, including professionals who should know better, to […]
[…] […]
I read this post with great interest. I’m a clinician who struggled with increasing body mass and steady upward creep of HbA1c for years, unable to keep any of the diets I tried because of constant hunger. As a last resort I tried the Atkins diet, and lost over 50 pounds in a year. My most recent A1c was 4.8. I found by personal experimentation that I couldn’t stray far from induction without starting to regain, and later learned the term “ketogenic” for the diet that I actually eat. My ongoing frustration is that, when I discuss this possibility for A1c management with my patients, they are so indoctrinated in the concept of “good carbs” (as widely misunderstood) that they can’t hear a word that I say. So they continue to eat whole-wheat bagels and brown rice and potatoes “including skins,” convinced that they are doing the best thing possible for their diabetes, while their clinical picture slowly deteriorates. Sorry to say that many colleagues are equally resistant. Maybe one day this evidence-based diet will be better understood. It may not be for everyone, but for those willing to keep it, the benefits may be extensive. I have been following with great interest the line of research on glucose metabolism days regulation in neurodegenerative diseases.
Keep writing. I will be following with keen interest.
wooddogs3, don’t be frustrated. While Atkins clearly works for weight loss and blood sugar control (first book is best!), it can be a pretty steep learning curve for many. For those who can’t imagine giving up their good carbs, I’d suggest the Lutz/Allan book, “Life Without Bread.” That program allows the persons doing the diet to choose their own carbs (including bread), and suggests how to limit those carbs to about 70-75 grams a day. While the results might not be as spectacular as what can be achieved by doing Atkins, the program does work.
Yes. There are many ways to take advantage of benefits of carbohydrate restriction. One of my daughters used to use what she called “Atkins-plus” which was a low-carb diet that included one Haagen-Dazs bar a day. As she put it: “A diet where Haagen-Dazs is equal to a grapefruit. That’s for me.” Of course, if you allow for carbs, you have to count things, e.g. if you use flour to coat things for frying, you have to measure (1 cup = 100g. 1/8 cup enough for a few cutlets or fish = 12.5 g which is not much per cutlet). On the other hand, one advantage of just cutting out obvious carbs is that you don’t have to think about food all the time. As for wooddogs3’s patients, you can ask them what I ask my medical students: “do you think that there’s ever been a time in the history of medicine where majority of physicians and scientists were totally wrong but refused to face the truth?” You can then ask them to consider that this night be another such time.
Thanks, both of you. New resources and new ways of approaching the issue and offering motivation are always appreciated. My own ongoing success is also a factor to some patients in a way that I hadn’t realized. One of them said to me recently “I saw you lose a lot of weight, and I wasn’t impressed because I’ve done that too. But now I’ve seen you be thin for two years and I’m impressed, because I’ve never done that. Let’s talk some more about those carbs.”
I like your daughter’s Atkins-plus idea, though I’d go for a measured amount of their ice cream. 🙂
Dr. Feinman wrote: “Of course, if you allow for carbs, you have to count things, e.g. if you use flour to coat things for frying, you have to measure (1 cup = 100g. 1/8 cup enough for a few cutlets or fish = 12.5 g which is not much per cutlet).” Actually, LWB doesn’t fiddle like that. They suggest that “small amounts of breading and sauces don’t count. . .” (pp. 5-6), though larger amounts, especially of sugar based sauces, such as barbeque sauce, would need to be counted. It really doesn’t take long to identify how much of frequently-used foods constitutes a bread unit. Aside from milk, which is a handy 12 carbs, I don’t measure things much any more. I learned long ago that there is no such thing as an exact count for a food item, anyway; the values given from one database to another for the same amount of the same food can vary widely. My understanding is that even for heavily processed packaged items, there is allowance for something like a 10% error.
Anyway, I’m off my original track, which was to suggest that, because it offers wider variety, something like Lutz/Allan might be a useful low-carb program for those aren’t ready to do Atkins induction.
“measured amount” sounds like portion control. I actually think that if there is anything to glycemic index, which is questionable, it is that ice cream is not so bad on low-cab diet, but unfortunately, for me, a portion of ice cream is the size of the container that it is in.
Dr. Feinman wrote: “. . .for me, a portion of ice cream is the size of the container that it is in.”
Thanks for a laugh. Yes. I was going to write “measured amount of [my favorite flavor],” but it’s been so long since I’ve dared have a container of ice cream in the house, I couldn’t remember what flavors there are, much less my favorite.
I think Dr. Bernstein has a recipe for butter pecan ice cream that doesn’t look too bad. I might try that some time.
On imitation carbs, I follow the advice of my old thesis advisor who would not smoke marijuana because he said it might lead him to the hard stuff by which he meant cigarettes.
Buy Dixie cups, if they still make those. If I ate any amount of real ice cream, I’d then rush out to the store through rain, sleet, and snow to get more, and I’d have to replace my wardrobe with beachball-shaped garments.
Having some problem with my own wardrobe but may have to go out to look for Dixie cups. I wonder if the lid still has pictures of movie stars. I know somebody who has a double and will trade his Lana Turner.
Wouldn’t it be possible to make ice cream with FOS, honey for instance so that you’d also get the benefit of resistant starch and thus help your beneficial little animals down there
I’m sure it’s possible. And we heard it here first. Good luck.
I haven’t tried anything as tempting as ice cream with imitation carbs. I do find them very useful for things like yogurt or coffee or a nut bread that I’ve just discovered. Since I find non-nutritive sweeteners (I only use stevia, erythritol and saccharin) far superior to sugar, which I now find icky and non-satisfying, there’s little chance of their leading me to the “hard stuff.”
I know Jeff Volek makes ice cream with erythritol and recipe is probably in Art and Science but I have not tried it.
Guys, I have here a fab recipe for LC ice cream, that basically came from Dr Peter Attia’s website. It is delicious and tastes so naughty it’s hard to beleive it isn’t!! You need an ice cream maker for it – one of the best buys of kitchen equipment I ever made!! Here you go
Keep all ingredients in the fridge until right up to the time you need them
Sorry the measurements are all mixed up UK/US)
3-5 cups double cream
or 1 tub (300ml) extra thick cream and 1 300ml tub double cream
2 egg yolks
2 desert spoons of granulated splenda and 2 desert spoons zylotol
2 dsp vanilla essence (make sure it’s not sweetened type – the real stuff!!)
1 cup unsweetened almond milk –
blend all together with electric whisk for a minute or so and pour into your ice cream maker.
Honestly the quantities can be fined tuned to your tastes, less or more sugar, essence, cream, eggs etc. But it’s fab. Never lasts long enough!! So if you ever have an urge, or want to prove to someone low carb needn’t mean a life of deprivation…. this is it.
Thanks! I’ve copied it. Now if I can only find the research I did on the best ice cream maker to buy. . . . 🙂
No I was never told about a low carb diet. The dietician who visited us in hospital said there is no such thing as a diabetic diet and you can eat whatever you like, even McDonalds. So I embarked on my own research and totally overhauled our whole family’s diet. It is through my own self education that I have achieved such excellent results with my son. And no, he rarely has hypos and his HbA1c is 5.5
You could send this to ADA or leave a comment on their site. They will undoubtedly say how much they believe in “individualization.”
Actually the most recent ADA position paper that came out last October states now, for the first time, that there is no one optimal mixture of macronutrients ie fat, carbohydrate, protein for diebetics. They also cite, on page 8, left most column, that there are studies that suggest that low carb diets have favorable effects on lipid profiles and list low carb diets as a possible option for diabetics.
Click to access dc13-2042.full.pdf
Nutrition Therapy Recommendations
for the Management of Adults
With Diabetes
ALISON B. EVERT, MS, RD, CDE1
JACKIE L. BOUCHER, MS, RD, LD, CDE2
MARJORIE CYPRESS, PHD, C-ANP, CDE3
STEPHANIE A. DUNBAR, MPH, RD4
MARION J. FRANZ, MS, RD, CDE5
ELIZABETH J. MAYER-DAVIS, PHD, RD6
JOSHUA J. NEUMILLER, PHAR
I cited this in the post (reference 1). As I mentioned, it is not clear what “optimal” means. Perfect? Is there any recommendation that is optimal in medicine? What they recommend is that people with diabetes have the level of protein and fat recommended for people without diabetes. That leaves a recommended level of carbohydrate. Is that optimal? If not, what is it? Default? That’s what we say low carb is. The default. So, does there individualization include low-carb is there only individualization within the range of their recommended diet which is the same as the recommendation for people without diabetes. The benefits of low-carb have been cited in their guidelines but have never influenced their recommendations and low-carb diets do not fit in with the level of fat recommended for population at large which they think is desirable (optimal?)
But I don’t understand your comment. Are you saying that the 2013 guidelines are a serious, intellectually sophisticated attempt to analyzed all the data and come up with a reasonable set of ideas that can help physicians and patients? If you have patients with diabetes, how does their analysis fit in with your practice? And do you have the sense that the authors are really experts? Insofar as these recommendations influence medical practice, do you think that they should be held accountable in any way?
I see it as a move in the right direction from their last position which was to endorse the AHA’s 30% calories from fats and 50 to 55% from carbohydrates guidelines, again a rigid fixed macronutrient mixture. It certainly isn’t an endorsement of low carb high fat which clearly is best for diabetics as Eric Westman, MD uses to treat his diabetics at Duke University. But at least they now leave the door open for those who want to recommend the diet without condemning it as “dangerous” and “unproven” they did in the past, when Robert Atkins him self advocated it.
They do not leave the door open because they do not recommend anything and therefore their previous recommendations are likely to be the ones that dietitians follow.
Here’s what they say about diet patterns “A variety of eating patterns have been shown modestly effective in man- aging diabetes including Mediterranean-style, Dietary Approaches to Stop Hypertension (DASH) style, plant-based (vegan or vege- tarian), lower-fat, and lower-carbohydrate patterns (36,46,72,92,93).”
The references for “lower-carbohydrate patterns:”
36. Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in in- dividuals with type 2 diabetes. Diabetes Care 2006;29:1777–1783
46. Azadbakht L, Fard NR, Karimi M, et al. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 di- abetic patients: a randomized crossover clinical trial. Diabetes Care 2011;34: 55–57
72. Esposito K, Maiorino MI, Ciotola M, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly di- agnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009;151:306– 314
92. Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus con- ventional weight loss diets in severely obese adults: one-year follow-up of a 103a. randomized trial. Ann Intern Med 2004; 140:778–785
93. Turner-McGrievy GM, Barnard ND, Cohen J, Jenkins DJ, Gloede L, Green AA. Changes in nutrient intake and dietary quality among participants with type 2 diabetes following a low-fat vegan diet or a conventional diabetes diet for 103b. 22 weeks. J Am Diet Assoc 2008;108: 1636–1645
Does this sound like good support for even a “lower-carbohydrate” diet? Low-carbohydrate is not even included. Does this sound like an honest mistake? After all, the literature is large. It’s hard to get all your references exactly right. Simple mistake. Right?
I’m afraid I disagree with your assessment. If this is a step in the right direction, what would waffling and avoiding the issue look like?
Probably so. It seems the only country willing to support low carb high fat in an official way is, of course, Sweden. We won’t be ready to here for a long time I’m afraid. The closest any US official body will come will be to endorse the “Mediterranean” diet, which I see as a cop out. In the recent study from Spain which showed hard outcomes benefits, the intervention was to eat 2 oz of olive oil or equivalent calories of nuts per day vs the control which ate low fat (and hence a high carb diet). The intervention group was also instructed to limit sweets and refined carbohydrates. Eat whole grains etc. The intervention group was essentially a higher fat lower carb diet compared to the control. I believe there is nothing magic about olive oil or nuts. They provided about 400 of the 2400 calories they ate which then replaced carbohydrates. I believe they could have substituted saturated fat or at least animal fat ie beef or pork (which is 50% monounsaturated fat anyway) in the study and gotten the same or better results. However, that would never be done, since it goes against the AHA’s 50 year old dogma to limit animal and saturated fats. I believe the official US organizations will endorse “Mediterranean” diets more and more praising the magic of olive oil and nut provided monounsaturated fats along with “wholesome whole grains and fruits” without ever putting it to the test against animal or saturated fats so not to challenge the misguided advice that has been given for the past 50 years to limit dietary cholesterol and saturated fat at the expense of consuming more metabolic syndrome, obesity, diabetes, cardiovascular disease causing carbohydrates. They seem to be slowly moving to discourage consumption of sugar as well, but that is probably as far as they will be willing to go for a long time.
Seems like we should not continue to accept it.
I’ve had to fight with every hospital dietitian I have had to work with after I order “Atkins induction <20 gm carb/d diets for my obese diabetic patients. In my current hospital we had to reach a compromise and allow fruit. I'll have to work on that later. My other big beef is nutritional supplements. Ensure is basically low fat milk with vitamins plus 30 more grams of carbohydrate. Glucerna, for diabetics, is the same ie low fat milk, vitamins ,plus 17 more grams carbohydrate. I tell my patients to drink whole milk for nutritional supplement. I never, ever order "heart healthy, low fat, low cholesterol" diets for my hospital patients. Basically, I order the same low carb diet for all my diabetics. I order the same diet for my cardiac patients after instruction on metabolic syndrome and pre diabetes, since nearly all cardiacs have metabolic syndrome which is CAUSED by the AHA recommended high carb low fat diets.
I don’t understand why somebody doesn’t simply yes Glucerna, Ensure, etc. against an Atkins shake. Whereas this is not recommended as a staple, it seems like a reasonable comparison.
It is UNbelievable what hospitals feed diabetic patients. It’s all about low fat. And if you happen to be on a cardiology floor, it’s salt-free, too.
It’s real. You better believe it.
I know. I’ve been getting reports from a friend.
Marilyn, what if you simply refuse to eat that stuff? I was in a research study that required admission to Brigham & Women’s. I said I was on a LC diet, but for the first meal, they included a HUGE slice of bread. They had to provide an exact number of calories, and that was probably an easy way to do it. I simply didn’t eat it, and bread didn’t appear again.
At B&W, it was rather easy to get a LC meal as they had menus, although they mostly had carby choices. I had poached salmon, broccoli, and salad, rejecting the sweet balsamic vinegar. If you were there for a week, you’d be eating a lot of salmon, which alternated with chicken on the menu. Not a lot of rib roasts.
They wouldn’t let me leave for the 3-hour drive home until my blood sugar was over 140 (they’d been doing a clamp study that involved infusing a lot of insulin) and asked what I’d eat. I asked for an apple. Would you believe a hospital kitchen would have no apples? I ended up eating a sweet yogurt, and they handed me some packaged peanut butter crackers. I read the label and asked why they were giving diabetic patients crackers that were full of trans fats (this was some time ago). The doc in charge agreed with me, but I doubt the dieticians changed their ways. I threw the crackers away.
If you’re hospitalized, you have to look out for yourself when you can. If you refused to eat the standard breakfast of OJ, cereal with skim milk, toast with jam and low-fat axle grease, I suspect they’d find something else. Some people will eat whatever you put in front of them.
Makes me very sad and uncharacteristically speechless.
I have type 3 DM and eat-to-the-meter. Last year I had a total knee replacement. I had a pretty good idea what I would be in for when it came to food. So besides my clothes and fragrance-free toiletries I packed a bag with butter (in a jar), coconut oil, olive and avocado oils, salt and single serve containers of bone broth and a small jar of mayonnaise. So then I ate whatever protein they sent and the low carb veggies, with the salt and fats I brought with me and left all the carby stuff (including the glucerna) on the tray. Can’t say it was wonderful but I managd to keep my blood glucose under 140mg/dL which is about all I could hope for. The “hospitalist” whatever that is came in and scolded me for testing too much. He insisted 4 times a day was enough. I tested before and 1 and 2 hours after meals. Didn’t cost him or the hospital anything. I brought my own meter and strips.
My “friend” aka my husband is coming home tomorrow and I’ll feed him in the manner to which he is accustomed. He had menus at the hospital from which to choose, and made the best choices he could, but refusing to eat the carbs that came along with the bit of protein served would have left him quite hungry. He asked for whole milk one day, and was told they didn’t have that. He’s been there less than a week, thank goodness, so we’ll put the matter behind us and get back to “healthy eating.” 🙂
Bon appétit.
Merci! He told me last night how good it was not to have lean dry meat for dinner. 🙂
Loved the article and loved the comments. Heartbreaking and heartwarming at the same time. Thanks for all the info, and we will just keep plugging away, knowing we are doing the right thing. This is my 14th year LC, except for Xmas, holidays and birthdays LOL. Luckily I’m not diabetic, but just feel great living and eating this way. My heart goes out to all the diabetics who are not served by the Diabetes organisations in any country – my dad is T1, 78 and virtually immobile. His faculties are gradually declining too as part of it (‘A’ level chemistry teacher) but can I get my mother to change his diet – in all these years – NO!! Thanks Drs, dieticians and nurses, you have condemned him to a slow and miserable death.
I am very sorry about this but we are trying to change things.
“Are we in agreement?”
I would agree with the restatement with one qualification: children. Young children will eat whatever you give them, or whatever the family is eating, but I think it would be very difficult for a teenager to follow a strict LC diet when all his/her friends were eating pizza. So maybe a temporary adjustment during what are pretty difficult years even without diabetes.
I was discussing the basic principles. On the practical application, you are the expert. As the talk-show hosts say: The book is “The First Year. Type 2 Diabetes” http://www.amazon.com/The-First-Year-Essential-Diagnosed/dp/1569242658 Gretchen Becker.
Let me first state I am always delighted when professor Feinman comes with a new post and if waited long enough for all the comments to appear I usually don’t have much to add. However there is one thing that is beginning to irk me a bit and that is this constant hammering on a pizza. I cannot for the life of me see how a pizza is so extremely high carb. A thin crust, a layer of tomato and herbs sauce, a layer of mushrooms, pepperoni, cheese, and topped off with bell peppers and a sprinkling of bacon. There are variations of course but the basis remain. Most of the carbs are of the good variety, fair bit of soluble fiber.
Thanks for the comments but I don’t hammer on pizza. Whether and, in what way you eat pizza, depends on who you are. If you don’t have a weight problem, you know how to eat pizza. If you do have a weight problem, you have to make it fit into your overall plan which may mean eating the top off if you are in a friendly crowd, or, like me, just eating the part of the bread that you left on to hold the rest of the slice. If you have diabetes or metabolic syndrome you eat to the meter, whatever doesn’t have adverse effect on your blood sugar. Now, that is what I say. Inside my head, however, is a little Lewis Black saying “You got diabetes…you don’t fucking get any pizza.”
Or when I lived in Iowa, one could get a ham and sauerkraut pizza. 🙂 The last locally made pizza we had around here got us a pretty high meter reading. I think they’ve cost-reduced what used to be a very good product. The tomato sauce is now noticeably sweeter, and the meat bits are really dinky.
Ham and sauerkraut pizza? I get agita just from the idea. But yes, cost reduction on good products once they start to sell. Pepperidge Farm turnovers used to be outstanding but as soon as they became popular, they changed the formula.
The only reference to pizza I saw on this post was made by me, so don’t blame Richard. In fact, most people with diabetes have noticed what we call “the pizza effect.” When you eat carbs plus fat, the blood sugar stays elevated for many hours. See http://tinyurl.com/pjsnv2c
I think this phenomenon was first discovered in nondiabetic healthy Yale undergrads, so it probably occurs in everyone. (Can’t locate that reference.)
But I think it’s a good illustration that a high-fat diet makes you more susceptible to the blood sugar raising effects of carbs, so you shouldn’t try to mix them.
Dr. Feinman,
I sent these question to Dr. Volek after listening to several of his lectures, but now I’m embarrassed because they are likely simplistic and he may be offended( I’m actually hoping my email gets rejected by one of his staff!). I am hoping to get an answer from you, since you were very approachable with my previous queries…..
1) I understand the effects of high insulin levels on the adipocyte, you have explained it well, with increase LPL activity and FA movement into the adipocyte. However, when the obese person is insulin resistant, the circulating high insulin levels would have a lessened effect on the fat cells. In that circumstance, I would envision fat efflux out of the adipocyte, not continued storage of TAGs. This should limit total fat mass, but then my logic breaks down and I ask myself where does all of the excess energy go? I know my thought process is errant, your explanation will be appreciated.
2) Re – fatty acid stored in TAGs in the adipocyte – are they mostly palmitic acid (ie saturated) or palmitoleic acid (ie monounsat) – I ask because I was confused by a comment that Dr. Phinney made during a podcast featuring both of you, something to the effect that the major fat in the body is monounsat. When HSL liberates FFAs from TAGs in the adipocyte and sends them out into the circulation with albumen, ie NEFAs, are those FFAs primarily palmitate or palmitoleic acid?
But my more pressing question is a theoretical one, an evolutionary thought – if ketosis is the metabolic state in which we were meant to exist, why is it that the body kicks us out of ketosis at the least “infraction” of CHO? Perhaps ketosis is only a fall back position, never meant for a 24/7 internal environment, and my type 2s would be better served with moderate reduction in CHO and being thereby fat adapted(sometimes using CHO for energy, but usually relying on beta oxidation), rather than flipping the switch to perpetual ketone production. Could ketosis be a low grade stressor, with poorer long term (decades later) outcomes? I’ve been reading about reports of ketosis-related health issues on some other blogs, I’d like to hear your thoughts.
Thank you so much for your input
Answer (of sorts) to Part 1) You are appropriately modest because the idea is out there that we understand all of this which we don’t. People have acted as if we’ve got it all worked out in the metabolic charts. The single area of lack of understanding is that all of these processes are time dependent and there are two major considerations. First, in a rough sort of way all processes have two things, the inputs and the rate of use. Second, everything is connected in feedback. So on your question, overall insulin resistance in adipocyte will protect against further obesity by slowing the process of fat storage but it isn’t shut down and over time, if you have a lot of TAG-rich lipoproteins you may continue to store fat. The fatty acid that is released may be used in other tissues and may cause further insulin resistance. The system continues to sense glucose and other things, howeverm and will release more insulin which may compensate for the insulin resistance. (Once you exceed the capacity of this feedback loop, you may have frank diabetes). The real answer is that I don’t think that we have enough information for grand explanations.
On the second question, I don’t now about different tissues. I will describe later the fatty acid distribution in plasma. Palmitoleic acid is a minor component. The major MUFA in humans is oleic acid (18:1 n-9, 18 carbons, one unsaturation at carbon 9) which derives from stearic acid, one of the major saturated fats (18:0) although palmitate (16:0) is also one.
On the third question:
if ketosis is the metabolic state in which we were meant to exist, why is it that the body kicks us out of ketosis at the least “infraction” of CHO?
I don’t think that we were meant to do anything in particular. The selective advantage in being able to use different fuels to cope with different environments goes back before humans. And whereas whole body ketosis responds in big ways, getting kicked in and out, its importance in local areas, for example in the brain, is just beginning to be explored.
Perhaps ketosis is only a fall back position, never meant for a 24/7 internal environment, and my type 2s would be better served with moderate reduction in CHO and being thereby fat adapted(sometimes using CHO for energy, but usually relying on beta oxidation), rather than flipping the switch to perpetual ketone production.
Again, while the selective advantage in being able to live on carbohydrate when available reflects something about the co-evolution of the species and its plant environment, I don’t think anything was “meant” to be. I don’t think we understand metabolism or, especially, its evolutionary driving force, to allow you to come up with a best diet. All we really know is that, overall, low carbohydrate will help your type 2s. The idea that it is not only the reduction in carbohydrate but the specific benefit of the ketone bodies is just beginning to be looked at but, right now, the questions out way the answers.
Could ketosis be a low grade stressor, with poorer long term (decades later) outcomes? I’ve been reading about reports of ketosis-related health issues on some other blogs, I’d like to hear your thoughts.
Anything could happen long term but since, unlike the witches in Macbeth, I cannot look into the seeds of time and say which grain will grow and which will not, I have to say again that I don’t know. I would be glad to consider the “ketosis-related health issues” of other bloggers but I don’t know of any myself.
“People have acted as if we’ve got it all worked out in the metabolic charts.”
I think this is an important, and wise, point. Too many diet gurus write/talk as if all our problems are caused by a single nutrient and we can fix everything by following their diet or buying their expensive supplement. Life is more complex than that.
That’s why I think Richard’s idea of LC diets as the “default diet” is the best approach. Start with a LC diet and see if it has good results for a particular person. If it does, wonderful. If not, or if that person simply can’t stick to that regimen for some reason or reasons, then try something else.
Different people have different metabolisms and also different ways of applying the concepts of LC. Nothing will be best for everyone. I think LC is best for most people with metabolic syndrome (usually overweight) or diabetes.
Agree with that. Of course, professor is the job. Which means you describe the ten things you know as if they were just a few parts of your deep knowledge. Lustig is better at it than I am but I am pretty good and I do admit periodically that we don’t know much.
Thanks for the honest appraisal , it is so refreshing.
It is difficult to ask patients to make the changes if I can’t tell them “for sure” that it is safe in the long run. I can only tell them that they’ll likely lose weight, their metabolic parameters will improve, but it is still an uphill battle when one is defying the recommendations of medical bodies and nutritionists and diabetes educators alike.
I will stay on the journey of self education, and thank you for providing this forum to chat.
I didn’t understand your question which was general on the science which is still being explored. For your patients, there is little ambiguity (from my analysis of the science; I don’t have patients). The best treatment for type 2 diabetes is to start by lowering carbs as much as possible and, if the patient is on medication, reduce accordingly. As for defying recommendations, you do have to explain that the best and the brightest, at some time in history, have recommended milk for ulcers which were bacterial infections, blood letting, going to war in Vietnam, or Iraq, and there is this exchange:
RDF:Don’t you think that recommending carbohydrates for people with diabetes is one of the worst scandals in the history of medicine?
Jessica A. Feinman, MD: Remember, Dad. I’m a psychiatrist. We used to treat people by sticking an ice pick in their brain.
I’m not sure which question you mean?
I am 100% convinced that lower CHO is the way to go, and I tape articles and references to that effect on my exam room cupboards so that patients can read while they are waiting for me, at least introduce them to those ideas even if the appointment is about something else and we won’t be discussing diet at that visit.
BUT, any referral that I generate to DEC (diabetes education center) endocrinologist, cardiologist,etc, who still advocate high CHO leave the patients confused and consult letters back to me questioning my sanity – most emphatically from DEC (a mandatory referral for all new diabetics) and the cardiologists on the post MI patients. Still, I
deal with it, will talk to anyone who is willing to debate with me, I am caring less and less if I am viewed by my colleagues as a “fringe medicine” practitioner.
I just meant the general questions which were not framed practically. Practically “lower CHO is the way to go.” Your comments are very interesting and there is no reason why you could not write to members of the ADA committee who I mentioned and ask if “individualization” is for real and, if so, how come you have these problems. Be interested to hear the answer.
I don’t think the ADA has any interest in me, I am a Canadian physician. I have spoken with docs in my area who are involved with drafting guidelines, we disagree. I’ve been told I have cherry picked my data. My practical success stories are starting to trickle in, such as the T2dm fellow whom I saw yesterday, whose A1C came back at 0.055. When the docs at the top are not willing to change their tune, it leaves the patients, who are usually not in a position to judge, feeling uncertain (and perhaps they use this to avoid making a change which they perceive as very difficult). I open the dialogue with them, I leave articles for them to read while they’re waiting for me, then send them to websites where they can get additional information. Slow but steady.
The ADA definitely has no interest in you…until you send them your story and copy to me and, slow as they may be on somethings, they will realize we are documenting their intransigence. But fighting with them is not much fun and it looks like you are receiving gratification from your patient outcomes which is more positive…of course, you may actually change a head or two at ADA.
pjensenmd: I’ve been thinking about your suggestion to use whole milk as a supplement, rather than Ensure, etc. I decided to check out Ensure and Boost.
Ensure Plus – 8 fl. oz.
Calories – 360
Fat – 11 g
Carbohydrate – 50g
Protein – 13 g
Boost Plus – 8 fl. oz.
Calories – 360
Fat – 14.17 g
Carbohydrate – 45.35 g
Protein – 14.17 g
Then I checked out ice cream:
If I needed to gain weight, and wanted to ingest 45-50 g of carbohydrates in the process, I’d DEFINITELY go with something more fun — and higher calorie:
Haagen Dasz Classic Vanilla Ice Cream – 1 cup
Calories – 450
Fat – 36
Carbohydrate – 42
Protein 10
And compare the ice cream ingredients — cream, skim milk, egg yolks, vanilla extract — to the chemistry set of ingredients in Boost and Ensure.
On the nutrition facts web sites I checked, whole milk, with 4.6 g of saturated fat, is declared “high in saturated fat,” while Boost, with 2.835 g is “low in saturated fat.” A less than 2 gram difference. Go figure.
I am sure that Haagen-Dasz would also have least effect on blood sugar. Worth testing. Of course, a cup of ice cream might not do it for me. I am not sure that there is anything to the glycemic index but if there is it is ice cream.
I agree. Hagen-Dasz wins over Ensure Plus easily.
I agree. Haagen-Dasz wins over Ensure Plus to me.
Not much progress is being made. They are now proposing to consider glycemic control as the least important health issue to tackle. So diet and exercise were you can affect the most and even reverse diabetes is going to be largely ignore. If this recommendation are adopted by many physicians.
Shift away from glycemic control in diabetes treatment detailed
http://www.sciencedaily.com/releases/2014/02/140220112406.htm
Diabetes in Focus
Study: Sleep apnea during REM tied to poor glucose control in diabetes
Breathing pauses due to sleep apnea during the rapid eye movement phase of sleep were associated with worse long-term glucose control in type 2 diabetes patients, according to a study in Diabetes Care. The results underscore the importance of wearing a continuous positive airway pressure mask in such patients, researchers said. The New York Times (tiered subscription model)/Well blog
Thank you for your posts & this very enlightening conversation. A huge thank you!
Forgive my vocab errors and any ignorant phrasing, I’m just beginning my learning on this topic.
One comment/question – in reading here, it has been mentioned a couple times that eating fat with carbs results in BG levels remaining raised for extended time. Looking at that backwards, wouldn’t it suggest that a diet higher in fat would require even lower levels of carbs than a low fat diet?
I don’t really have a point, but was struck by the possibility that all the low fat recommendations of the last 50 years basically enabled an extremely high carb diet to degrade us a bit slower than it would have if more ‘normal’ levels of fat were consumed.
Certain levels of blood glucose are necessary, right? So more fat in the diet somewhat lengthens the effect of carbs therefor suggesting that carbs are the considered by the body as the scarcer nutrient? There wouldn’t seem to be any evolutionary advantage to enhancing a plentiful nutrient? Not sure if this makes any sense.
My thoughts on this are somewhat in trying to figure out the whole paleo orientation and its validity. I guess that also means trying to figure out a proper proportion of nutrients to aim for – trial and error makes me impatient!
“mentioned a couple times that eating fat with carbs results in BG levels remaining raised for extended time. Looking at that backwards, wouldn’t it suggest that a diet higher in fat would require even lower levels of carbs than a low fat diet?”
I don’t understand what you mean here.
“all the low fat recommendations of the last 50 years basically enabled an extremely high carb diet to degrade us a bit slower than it would have if more ‘normal’ levels of fat were consumed.”
I think that I agree with that.
“Certain levels of blood glucose are necessary, right? So more fat in the diet somewhat lengthens the effect of carbs therefor suggesting that carbs are the considered by the body as the scarcer nutrient? There wouldn’t seem to be any evolutionary advantage to enhancing a plentiful nutrient? Not sure if this makes any sense.”
Not sure what you mean but you do not need any carbohydrate to maintain blood glucose.
“My thoughts on this are somewhat in trying to figure out the whole paleo orientation and its validity. I guess that also means trying to figure out a proper proportion of nutrients to aim for – trial and error makes me impatient!”
I don’t know about Paleo but for most things from a therapeutic standpoint, weight loss, diabetes and metabolic syndrome, the fewer the carbs the better. That is the best way to start but every body has to do a certain amount of trial and error. I hope that helps.
Went to the ADA website to see what they are recommending to eat these days. The top 10 “superfoods” included whole grains, sweet potatoes, and yogurt. If you ate their 10 top in 1 day it would be 171 grams of carbohydrate.
They will probably tell you that that would be a reduction for many patients and it might but it is still not right.
[…] 2. American Diabetes Association Embraces Low-Carbohydrate Diets. Can You Believe It? | Richard David F… […]
Believe ADA? Never, ever.
Our society eats so much sugar …. Every sensible person knows that carbs are the culprit here.
[…] American Diabetes Association Embraces Low-Carbohydrate … – Recent Posts. Carrot Nation; American Diabetes Association Embraces Low-Carbohydrate Diets. Can You Believe It? Health risks of low-carbohydrate diets…. […]
[…] American Diabetes Association Embraces Low … – Recent Posts. Carrot Nation; American Diabetes Association Embraces Low-Carbohydrate Diets. Can You Believe It? Health risks of low-carbohydrate diets…. […]
A cut and paste from Mescape article of ‘nutrition for diabetes’
(Having just read your book ‘the world turned upside down’ I can now see the confusion. They recommend low fat, but then go on to say low carb provides better lipid control)
Begin quote:
Food groups include macronutrients and micronutrients. There is no optimal diet mix of macronutrients that can be prescribed to the entire diabetic population. Dietary needs must be individualized. Reduction in fat (saturated fats, trans -fats, cholesterol) intake in diabetic patients is aimed at decreasing cardiovascular disease risk by reducing plasma cholesterol and low-density lipoprotein (LDL) cholesterol levels.
Low-carbohydrate and low-fat diets used to achieve initial weight loss are effective for the short term (approximately 1 y) and need monitoring with a lipid profile and renal function tests.
Low-carbohydrate diets (20-120 g/d) carry the additional benefit of a favorable lipid profile as compared with low-fat diets. Low-carbohydrate diets have also been noted to decrease fasting plasma glucose values by about 21-28 mg/dL.[4]
The so-called Mediterranean diet may be an option. One study in which subjects (N=322) were randomized to 1 of 3 diets (Mediterranean, restricted-calorie; low-fat, restricted-calorie; low-carbohydrate, non–restricted-calorie) found that at 2-year follow-up, the 36 diabetic subjects assigned to the Mediterranean diet had more favorable fasting plasma glucose and insulin levels compared with those assigned to the low-fat diet.[9]
(no mention of comparison with low carb – I wonder why, i want to know! ?)
For patients who are on insulin therapy or oral hypoglycemics, being on a restrictive diet requires adjustment of dosage to prevent hypoglycemia.
Carbohydrate choices in diabetes are as follows:
Carbohydrates necessary for energy, some vitamins, fiber, and dietary palatability and as a major regulator of postprandial glucose levels
Recommended daily allowance for carbohydrates is 130 g/d[8]
Type of carbohydrates (ie, starch, amylose, amylopectin) consumed reflects on postprandial glucose values
Consumption of low–glycemic index foods can result in a drop of 0.4% in hemoglobin A1C compared with high–glycemic index foods[7] ; limitations to this diet choice include bloating and a restrictive diet
Nonnutritive sweeteners have fewer calories compared with regular sucrose used in table sugar but have not been shown to reduce glycemia, accelerate weight loss, or cause weight gain[10]
Dietary fat recommendations in diabetes are as follows:
Total dietary cholesterol consumption of less than 200 mg/d
Saturated fat intake consumption of a maximum of only 7% of one’s daily intake” (end quote)
So I am left confused. What does this mean? the non specified ‘mediterranean’ diet was better than a low fat diet, but that we should limit fat, however low carb is best?
Can someone make sense of this? Is the 130g carb what you talk about in your book as coming from what they assume the brain needs by way of glucose to function?
The obvious conclusion is that they are in a bind. They don’t know what they are doing. They don’t know how to back out of previous bad ideas. And the nutrition committee, in any case, are not eminent characters. There is such a thing as a really terrible document.
For the best part of a decade now, to my knowledge, the ADA have slated low carb diets “because there are no long term studies”. If they had started one ten years ago they would have had ten years of results. However they would probably have lost ten years of sponsorship.
During that decade, on their very own forum, as on most other diabetes forums and newsgroups, there has been a succession of success stories. Hundreds if not thousands of anecdotes remain anecdotes, while studies of small numbers of patients bought and paid for by the Sugar Bureau are “data”.
When John Buse was in charge they decided that low carb diets were permitted only for weight loss, not glycemic control, for a maximum of a year, and not lower than 135g carbs. The result was that some of their sponsors pulled their money, if I recall correctly General Mills and Cadbury Schweppes.
Most of these successes come from controlling peak postprandial blood glucose using this or similar techniques
http://loraldiabetes.blogspot.co.uk/2009/04/test-test-test.html
despite numerous requests this has never been subjected to a trial, not even the meter manufacturers and importers in many countries have shown any interest in sponsoring such a trial. Obviously no drug company, carbohydrate processor or margarine manufacturer would increase sales from such a trial, and since these are most of the sponsors not only of the ADA but the AHA, ADieteticA, and equivalent “charities” in most other countries, I predict no such trial will ever be funded.
Meanwhile have a look at the prices and side effects of some of the new “diabetes drugs” and gnash your teeth
This is a beautiful summary of the problem
Just looking at the most recent Nutritional Therapy Recommendations
http://care.diabetesjournals.org/content/36/11/3821.full
they list an A1c improvement in Type 2 of 0.5 – 2%
On their very own forum you will routinely see improvements of 5 – 8% and even over 10%.
Obviously they are studying the WRONG diet – and also the wrong patients – many studies exclude subjects with A1c below 8%, some only exclude subjects below 6.5%, very few include truly well controlled diabetics so doctors not only believe no such patients exist, they have no clue as to how they achieve these results – and since ACCORD many believe it is actually dangerous to reduce A1c below 6.5%. Well it is if you tell them to “eat more starch!” – a page which has finally gone from the ADA site – and follow up with heroic amounts of medication including TZDs, and some of the current meds look no less risky.
Here in the UK our “authorities” track the ADA by about ten years. The results speak for themselves – less than 10% of Type 1s and a quarter of Type 2s have A1c below 6.5%, three quarters of Type 1s and a third of Type 2s have A1c over 7.5%. These numbers have been largely the same for a decade, except that far more diabetics have been diagnosed, and since no-one was sacked for gross incompetence this outcome must be intended. Even if your original post was to come true the slaughter will continue here and no doubt in other countries, unless and until The Establishment notices what is occurring at the grassroots with increasing numbers of researchers and clueful doctors.
Chris C, I think this statement from the Nutritional Therapy Recommendations pretty much says it all: “Due to the progressive nature of type 2 diabetes, nutrition and physical activity interventions alone (i.e., without pharmacotherapy) are generally not adequately effective in maintaining persistent glycemic control over time for many individuals.”