(Answers to last week’s organic puzzler at the end of this post).
One of the more remarkable results from Jeff Volek’s laboratory in the past few years was the demonstration that when the blood of volunteers was assayed for saturated fatty acids (SFA), those subjects who had been on a very low-carbohydrate diet had lower levels than those on an isocaloric low-fat diet. This, despite the fact that the low-carbohydrate diet had three times the amount of saturated fat as the low-fat diet. How is this possible? What happened to the saturated fat in the low-carbohydrate diet? Well, that’s what metabolism does. The saturated fat in the low-carbohydrate arm was oxidized while (the real impact of the study) the low-fat arm is making new saturated fatty acid. Volek’s former student Cassandra Forsythe extended the idea by showing how, even under eucaloric conditions (no weight loss) dietary fat has relatively small impact on plasma fat.
The essential point of what I now call the Volek-Westman principle — we should be speaking of basic principles because the idea is more important than specific diets where it is impossible to get any agreement on definitions — the principle is that carbohydrate, directly or indirectly through insulin and other hormones, controls what happens to ingested (or stored) fatty acids. The motto of the Nutrition & Metabolism Society is: “A high fat diet in the presence of carbohydrate is different than a high fat diet in the presence of low carbohydrate.” Widely attributed to me, it is almost certainly something I once said although it has been said by others and the studies from Volek’s lab give you the most telling evidence.
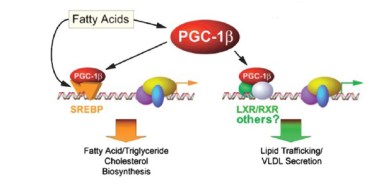 The question is critical. Whereas the scientific evidence now establishes that dietary saturated fat has no effect on cardiovascular disease, obesity or anything else, plasma saturated fatty acids can be a cellular signal and if you study the effect of dietary saturated fatty acids under conditions where carbohydrate is high and/or in rodents where plasma fat better correlates with dietary fat, then you will confuse plasma fat with dietary fat. An important study identified potential cellular elements in control of gene transcription that bear on lipid metabolism.
The question is critical. Whereas the scientific evidence now establishes that dietary saturated fat has no effect on cardiovascular disease, obesity or anything else, plasma saturated fatty acids can be a cellular signal and if you study the effect of dietary saturated fatty acids under conditions where carbohydrate is high and/or in rodents where plasma fat better correlates with dietary fat, then you will confuse plasma fat with dietary fat. An important study identified potential cellular elements in control of gene transcription that bear on lipid metabolism.
So, it is important to know about plasma saturated fatty acids. First, recall that strictly speaking there are only saturated fatty acids (SFA) — this is explained in detail in an earlier post. What is called saturated fats simply mean those fats that have a high percentage of SFAs — things that we identify as “saturated fats,” like butter, are usually only 50 % saturated fatty acids (coconut oil is probably the only fat that is almost entirely saturated fatty acids but because they are medium chain length, they are usually considered a special case).
In Volek’s study, 40 overweight subjects were randomly assigned either to a carbohydrate-restricted diet (abbreviated CRD; %CHO:fat:protein = 12:59:28) or to a low fat diet, (LFD; %CHO:fat:protein = 56:24:20). The group was unusual in that they were all overweight would be characterized as having metabolic syndrome, in particular they all had, atherogenic dyslipidemia, which is the term given to a poor lipid profile (high triacylglycerol (TAG), low HDL-C, high small-dense LDL (so-called pattern B)). Metabolic syndrome (MetS) is the predisposition to CVD and diabetes and is characterized by the constellation of overweight, atherogenic dyslipidemia and, by now, a dozen other markers.
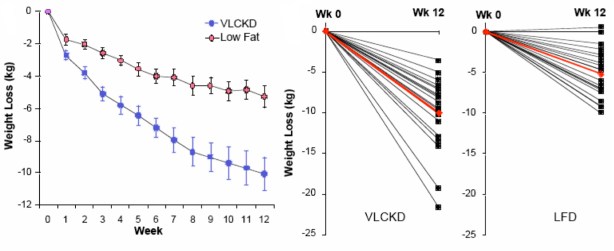
The paper is one of the more striking for the differences in weight loss between two diet regimens. Although participants were not specifically counseled to reduce calories, there was a reduction in total caloric intake in both two groups. The response in weight loss, however, due to the difference in macronutrient composition, was dramatically different in the two groups. The CRD group (labelled as very low carbohydrate ketogenic diet (VLCKD) in the figure) lost twice as much weight on average as the low-fat controls despite the similar caloric intake. Although there was substantial individual variation, 9 of 20 subjects in the CRD (VLCKD) group lost 10% of their starting weight. more than that lost by any of the subjects in the LFD group. In fact, nobody following the LFD lost as much weight as the average for the low-carbohydrate group and, unlike George Bray’s demonstration of caloric inefficiency, whole body fat mass was where the major differences between the CRD (VLCKD) and LF appeared (5.7 kg vs 3.7 kg). Of significance is the observation that fat mass in the abdominal region decreased more in subjects on the CRD than in subjects following the LFD (-828 g vs -506 g). This is one of the more dramatic effects of carbohydrate restriction on weight loss but many have preceded it and these have been frequently criticized for increasing the amount of saturated fat (whether or not any particular study actually increased saturated fat). Although the original “concern” was that this would lead to increased plasma cholesterol, eventually saturated fat became a generalized villain and, insofar as any science was involved, the effects of plasma saturated fat were assumed to be due to dietary saturated fat. The outcome of Volek’s study was surprising. Surprising because the effect was so clear cut (no statistics needed) and because an underlying mechanism could explain the results.
Saturated Fat
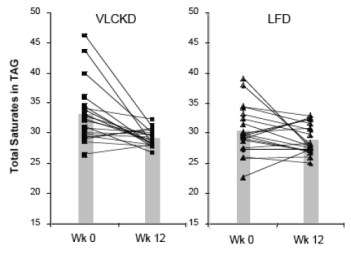 The dietary intake of saturated fat for the people on the VLCKD (36 g/day) was threefold higher than that of the people on the LFD (12 g/day). When the relative proportions of circulating SFAs in the triglyceride and cholesterol ester fractions were determined, they were actually lower in the low carb group. Seventeen of 20 subjects on the CRD (VLCKD) showed a decrease in total saturates (the others had low values at baseline) in comparison to half of the subjects consuming the LFD had a decrease in saturates. When the absolute fasting TAG levels are taken into account (low carbohydrate diets reliably reduce TAB=G), the absolute concentration of total saturates in plasma TAG was reduced by 57% in the low carbohydrate arm compared to 24% reduction in the low fat arm who had, in fact, reduced their saturated fat intake. One of the saturated fatty acids of greatest interest was palmitic acid or, in chemical short-hand, 16:0 (16 means that there are 16 carbons and 0 means there are no double bonds, that is, no unsaturation).
The dietary intake of saturated fat for the people on the VLCKD (36 g/day) was threefold higher than that of the people on the LFD (12 g/day). When the relative proportions of circulating SFAs in the triglyceride and cholesterol ester fractions were determined, they were actually lower in the low carb group. Seventeen of 20 subjects on the CRD (VLCKD) showed a decrease in total saturates (the others had low values at baseline) in comparison to half of the subjects consuming the LFD had a decrease in saturates. When the absolute fasting TAG levels are taken into account (low carbohydrate diets reliably reduce TAB=G), the absolute concentration of total saturates in plasma TAG was reduced by 57% in the low carbohydrate arm compared to 24% reduction in the low fat arm who had, in fact, reduced their saturated fat intake. One of the saturated fatty acids of greatest interest was palmitic acid or, in chemical short-hand, 16:0 (16 means that there are 16 carbons and 0 means there are no double bonds, that is, no unsaturation).
So how could this happen? The low fat group reduced their SFA intake by one-third, yet had more SFA in their blood than the low-carbohydrate group who had actually increased intake. Well, we need to look at the next thing in metabolism.
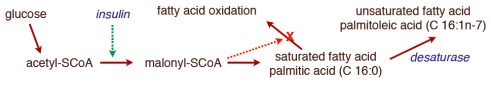
In the post on An Introduction to Metabolism, we made the generalization that there were roughly two kinds of fuel, glucose and acetyl-CoA (the two carbon derivative of acetic acid). The big principle in metabolism was that you could make acetyl-CoA from glucose, but (with some exceptions) you couldn’t make glucose from acetyl-CoA, or more generally, you can make fat from glucose but you can’t make glucose from fat. How do you make fat from glucose? Part of the picture is making new fatty acids, the process known as De Novo Lipogenesis (DNL) or more accurately de novo fatty acid synthesis. The mechanism then involves successively patching together two carbon acetyl-CoA units until you reach the chain length of 16 carbons, palmitic acid. The first step is formation of a three carbon compound, malonyl-CoA, a process which is under the control of insulin. Malonyl-CoA starts the process of DNL but simultaneously prevents oxidation of any fatty acid since, if you are making it, you don’t want to burn it. This can be further processed, among other things, can be elongated to stearic acid (18:0). So this is a reasonable explanation for the increased saturated fatty acid in the low-fat group: the higher carbohydrate diet has higher insulin levels on average, encouraging diversion of calories into fatty acid synthesis and repressing oxidation. How could this be tested?
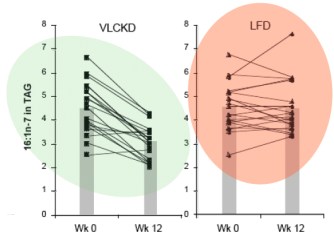 It turns out that, in addition to elongation, the palmitic acid can be desaturated to make the unsaturated fatty acid, palmitoleic acid (16:1-n7, 16 carbons, one unsaturation at carbon 7) and the same enzyme that catalyzes this reaction will convert stearic acid (18:0) to the unsaturated fatty acid oleic acid (18:1n-7). The enzyme is named for the second reaction stearoyl desaturase-1 (SCD-1; medical students always hate seeing a “-1” since they know 2 and 3 may will have to be learned although, in this case, they are less important). SCD-1 is a membrane-bound enzyme and it seems that it is not swimming around the cell looking for fatty acids but is, rather, closely tied to DNL, that is, it preferentially de-saturates newly formed palmitic acid to palmitoleic acid.
It turns out that, in addition to elongation, the palmitic acid can be desaturated to make the unsaturated fatty acid, palmitoleic acid (16:1-n7, 16 carbons, one unsaturation at carbon 7) and the same enzyme that catalyzes this reaction will convert stearic acid (18:0) to the unsaturated fatty acid oleic acid (18:1n-7). The enzyme is named for the second reaction stearoyl desaturase-1 (SCD-1; medical students always hate seeing a “-1” since they know 2 and 3 may will have to be learned although, in this case, they are less important). SCD-1 is a membrane-bound enzyme and it seems that it is not swimming around the cell looking for fatty acids but is, rather, closely tied to DNL, that is, it preferentially de-saturates newly formed palmitic acid to palmitoleic acid.
There is very little palmitoleic acid in the diet so its presence in the blood is an indication of SCD-1 activity. The data show a 31% decrease in palmitoleic acid (16:1n-7) in the blood of subjects on the low-carb arm with little overall change in the average response in the low fat group. Saturated fat, in your blood or on your plate?
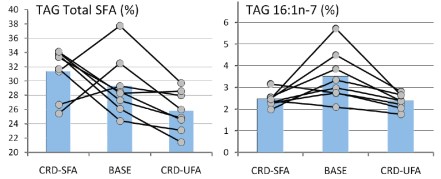
Forsythe’s paper extended the work by putting men on two different weight-maintaining low-carbohydrate diets for 6 weeks. One of the diets was designed to be high in SFA (high in dairy fat and eggs), and the other, was designed to be higher in unsaturated fat from both polyunsaturated (PUFA) and monounsaturated (MUFA) fatty acids (high in fish, nuts, omega-3 enriched eggs, and olive oil). The relative percentages of SFA:MUFA: PUFA were, for the SFA-carbohydrate-restricted diet, 31: 21:5, and for the UFA diet, 17:25:15. The results showed that the major changes in plasma SFA and MUFA were in the plasma TAG fraction although probably much less than might be expected given the nearly two-fold difference in dietary saturated fat and, as the authors point out: “the most striking finding was the lack of association between dietary SFA intake and plasma SFA concentrations.”
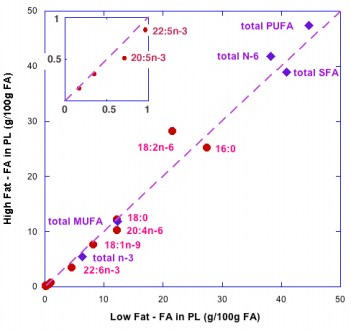
 So although it is widely said that the type of fat is more important than the amount, the type is not particularly important. But, what about the amount? A widely cited paper by Raatz, et al. suggested, as indicated by the title, that ‘‘Total fat intake modifies plasma fatty acid composition in humans”, but the data in the paper shows that differences between high fat and low fat were in fact minimal (figure below).
So although it is widely said that the type of fat is more important than the amount, the type is not particularly important. But, what about the amount? A widely cited paper by Raatz, et al. suggested, as indicated by the title, that ‘‘Total fat intake modifies plasma fatty acid composition in humans”, but the data in the paper shows that differences between high fat and low fat were in fact minimal (figure below).
The bottom line is that distribution of types of fatty acid in plasma is more dependent on the level of carbohydrate then the level or type of fat. Volek and Forsythe give you a good reason to focus on the carbohydrate content of your diet. What about the type of carbohydrate? In other words, is glycemic index important? Is fructose as bad as they say? We will look at that in a future post in which I will conclude that no change in the type of carbohydrate will ever have the same kind of effect as replacing carbohydrate across the board with fat. I’ll prove it.
====================================================================
Answers to the organic quiz.
Excellent post on the very important Westman-Volek Principle.
Does the higher proportion of palmitic and palmitoleic acids from DNL have medical significance, or would an equally high level of other SFA/MUFA fats be as bad?
What the study shows is that insofar as plasma saturated fat has medical significance, you will lower it better by restricting carbohydrate than restricting fat, saturated or total. I do not know what the effect of plasma saturated fat is in the big picture. Most studies have been done in animal or in vitro systems and I personally don’t have an opinion especially since I think it is fair to say that few workers recognize the limitations of especially rodent models in lipid metabolism. In many strains of mice, for example, a high-fat diet may have a major effect whether there is carbohydrate there or not.
What I like about Volek’s paper is that he shows not just averages but individual patient results. Although most patients may go up or down in some factor on some diet, a minority may do just the opposite, so people shouldn’t slavishly follow some diet just because the average person benefited.
Was the palmitoleic acid they found cis or trans? There’s trans in dairy foods.
Most naturally occurring fatty acids are cis as is the palmitoleic acid formed from the action of SCD-1. The trans-palmitoleic acid is in very low concentration in dairy and there was a paper a year ago saying that it had benefit for something or other but, if it meant anything is that it was an indicator of total fat which probably did have a benefit.
It was a paper saying people with more of the trans had lower rates of diabetes.
http://www.ncbi.nlm.nih.gov/pubmed/21173413
So I was surprised when Volek and Phinney suggested that POA predicts the development of diabetes.
I wonder where the cows get the trans form. Bacterial?
I don’t think that this paper made much sense. The level of trans-palmitoleic acid was very low and was directly proportional to the large amount of total fat so it was the total fat that correlated with reduced rate of diabetes if there was any. I haven’t gone back to the paper but I recall it was another reliance on epidemiology in place of common sense. There are more molecules in heaven and earth than are dreamt of in your philosophies. Cows may make this stuff for reason we don’t know yet but bacteria is possible too. POA?
Or from pasteurization at high temps?
POA = palmitoleic acid, Volek’s usage.
I think you’re correct that it’s the bacteria that produce the trans. Found this:
“These are products of the biohydrogenation of linoleic and linolenic acids from herbage by rumen microorganisms. In addition, monoenoic fatty acids with trans configurations have been detected in the membrane lipids of some aerobic bacteria, such as Pseudomonas putida, which have the capacity to synthesise them de novo. In this instance, trans fatty acids are synthesised in the cytoplasmic membrane by isomerization of the analogous double bonds of the cis configuration. Trans-9- and trans-3-18:1 are occasionally reported from seed oils. Otherwise, trans-18:1 isomers are only rarely encountered in natural lipids, although they are present in oils that have been hydrogenated industrially.”
Apparently at least some bacteria have isomerases, which they use when stressed. One theory is that stress like high heat increases fluidity of membrane, and conversion to trans helps to counteract that faster than de novo synthesis.
Not quite clear. Hydrogenation of linoleic acid will reduce the unsaturation. Commercial hydrogenation produces trans-fatty acid as a by-product. Isomerization can be part of other reactions. Most naturally occuring unsaturated fatty acids are cis- but in the process of oxidation they pass through a trans- stage.
The trans fats in dairy foods are beneficial, however, as far as anyone can tell. If the trans fat is made in a body and not in a factory (assuming no GMO involvement) then it’s looking like it’s harmless compared to the factory stuff, or even the stuff made at high heat on your stove out of vegetable oil.
The question is about trans-palmitoleic acid which I don’t think amounts to anything; see answer to Gretchen. I don’t know about other trans-fatty acids. Conjugated linoleic acid has one trans- bond and is generally considered good but I don’t know much about it off the top of my head.
[…] eucaloric conditions (no weight loss) dietary fat has relatively small impact on plasma fat. Read More […]
“…yet had more SFA in their blood than the low-fat group who had actually increased intake.”
Should be “low-carb group”?
Thanks. Fixed.
The study you cited to show the harmlessness of dietary saturated fat seems actually to conclude that replacing SFA with PUFA (but not MUFA or carbohydrate) reduces cardiovascular risk. I’m not saying I buy that, but does that study really support the idea that eating large amounts of SFA is harmless?
My interest is in part personal, since my doc is getting quite hinky about my (calculated) LDL of 217, despite my HDL of 157 and fasting TG of 39 on a relatively low carb, high SFA diet. You can guess his advice. I need ammunition!
What the Jakobsen study really showed is that there is no evidence for effect of dietary fat on cardiovascular disease and probably never was. I will explain further and provide real ammunition. Remember your doc does not have experience with any of this — how could he or she? Although CVD is a big killer, if you take 5,000 men for 5 years, there will be a small number of events. So they rely on the scientific literature…just like you and me. So I will provide more info on that literature.
Bill, have a listen to this podcast: http://www.askthelowcarbexperts.com/2012/02/8-what-questions-should-i-ask-my-non-low-carb-friendly-doc-dr-mary-vernon/
Explains why many doctors push the statins and other drugs, has to do with doctor ratings and not necessarily your doctor’s beliefs or training on the issue. Accepting the prescription paper and not actually filling it is a win-win in the current climate.
Cheers…
Your doctor’s belief may be real but not based on training in this issue. I would not assume, however, that the physician will be closed minded on the subject. Most physicians are not as doctrinaire as the nutrition panels from the health organizations.
Bill, you state you have HDL 157? You mean 57 right?
Nope, my HDL is 157. And it’s not a lab error since it’s in line with prior tests. Over the years, both HDL and LDL have gradually increased, with triglycerides dropping.
None of my docs has ever seen an HDL level anywhere near this high before. Highish HDL does run in my family, but no one is anywhere near this level. Now that the (calculated) LDL has surpassed 200, my primary care doc is getting rather hinky.
Your HDL is amazingly high. I have had similar discussions with my primary care doctor. Honestly, I only picked him out of a hat so I could get my full lipid profile, so I figured I’d get a run-of-the-mill doctor. However, it still did not prepare me when he told me that my profile was “abnormal”.
My first ever fasting profile on low-carbohydrate lifestyle was:
Total Cholesterol: 189
Trig: 50
HDL: 51
Chol/HDL Ratio: 3.7
LDL (Direct): 117
The doctor was concerned about my LDL levels. When I began to mention about particle size, he actually waved me off stating “No, no, no. It doesn’t matter.” The top of the lab results state:
“Your lipid profile is abnormal. Please continue to work on a low fat diet, exercise and weight management. Please return in 3 months.”
Now go into the future and I had another unexpected lipid profile due to some minor sinus surgery – and since it was unexpected I had a high fat lunch which launched my triglycerides into the stratosphere:
Total Cholesterol: 207
Triglycerides: 143
HDL: 57
Chol/HDL Ratio: 3.6 ratio
LDL (Direct): 126
From what I’ve read, triglycerides are normally the only major affected stat affected when having not fasted before the test. So, looks like my cholesterol went above 200, my HDL went up a bit, as did my LDL.
My doctor, seeing me for my pre-op was a bit concerned. I have passed the magical threshold of 200 for total cholesterol. He stated if it got any worse, I’d probably have to take medication. Furthermore, I’d have to avoid butter, cream, fatty foods, oil and red meat. I told him that is all I eat. Imagine the look on his face.
I did not argue with him. I simply left. What bothered me the most about this last encounter is that I know for a fact this doctor is giving this same advice to hundreds of unknowing patients. These patients then cut out fat further and introduce more carbohydrates into their diet, probably worsening their condition. Throw statins on top of that and they are in for a heap of trouble. Honestly, I don’t even think he’s even ever heard of type A LDL.
Back to you Bill – I’m still amazed by that number! Amazing HDL/Trig ratio!
Imagine the reaction I get with a total cholesterol approaching 400! Our experiences are similar, except that I’m dealing with a truly wonderful primary care doc I’ve known for several years. I want to keep a good relationship with him. It’s bad enough that I decline the PSA test and colonoscopy, and now I’m killing myself with fat!
It’s awkward of course, since I don’t want to appear to be questioning his professional knowledge or opinions. But I won’t go back to “healthy whole grains” or take a statin, so it creates a difficult situation.
Docs no longer seem to believe, as they once did, that a high HDL trumps the other “risk factors.” So even people like me, with stellar lipid profiles, BP, weight, fasting sugar and insulin, etc., but “high” LDL, get the usual lectures.
This is all too common Josh. I explained this to my doc who put herself on statins. She just won’t listen. It’s kinda creepy if you ask me.
“I will explain further and provide real ammunition.”
Thank you. This would be of great help to me, and to many others in the same boat, I’m sure.
I will put this together systematically but there is something inherently wrong with a meta-analysis of the type that Jakobsen did, where most of the studies showed nothing. So this type of meta-analysis is essentially adding a bunch of zeroes and coming up with a number which doesn’t make sense. I am not an expert on Bayesian analysis, the type of statistics where predictive ability of one study is affected by others but I think that is the analysis to apply. So, having a study that failed to show an effect, the next one should be strong to make you think that the errors were random rather than systematic. So, one of the personal questions you are asking is whether there is an effect of fat on diet and the answer is no. Not any type of fat. The different substitutions should not be pooled but, in some sense, multiplied. A bunch of failures is really bad and each reinforces the failure of the others. Does that make sense?
Yes, this does make sense to me. Such meta-analyses of equivocal studies seem highly questionable. If there really were a strong, clear effect, shouldn’t the individual studies reveal it? If pooling disparate data sets to torture out a “significant” finding is necessary, I have to wonder if there is really anything substantial to find. If there is, it must be very subtle.
The practical problem for people like me, as you know, is how to keep a good relationship with our docs when our LDL (or whatever else) is “out of range” and intervention is pushed. Some of what docs do really *is* valuable, and I know I’ll genuinely need his help one day. Plus, I do respect him. He certainly means well. I just can’t quite buy the supposed science he is relying on, as you said.
We laymen need an emergency doctor-mollifying lipid-panel-deflecting kit!
My first thought was to compromise and agree to an advanced lipoprotein test, on the assumption that it would show, say, a much more reassuring *measured* LDL-C, LDL-P, and Pattern A. But to be honest I’m not sure even those parameters have any clear practical significance. Does anyone really know? The various advanced lipoprotein tests don’t even seem to agree with each other very well.
Opinions are strong, but I seriously wonder if any of these tests, whether basic or advanced, are clearly supported by believable evidence that would justify, in the otherwise well at least, dietary or medical interventions that are not necessarily benign.
Ask, don’t tell. My experience is that most doctors are not particularly doctrinaire and will listen to an argument that TAG/HDL is supposed to be better than LDL. But you have the right to ask the American Heart Association about all these other markers, particle size, apoB/apoA1, etc. Ae these experimental? Are they to be disregarded? I never get an informative answer but you never know.
This article is helpful when considering studies and meta-analyses:
http://www.theatlantic.com/magazine/archive/2010/11/lies-damned-lies-and-medical-science/8269/
Thanks. A look at the recent paper on red meat would probably really make Iaonnides go crazy.
Bill, this is my opinion due to experiences thru many web sites. Triglycerides under 100 is very important. Your triglycerides are so low that I ( me personally ) would totally ignore the high LDL. It is the large fluffy , healthy kind. I am not a doctor but I doubt that he can prove me wrong.
Thank you!!! I’m too much of an illiterate about this stuff to discuss any specifics, but the basic information comes through loud and clear.
[…] Loss Diet PillsMy Paleo Kids are Hungry All The Time!!! Help!!!Am I eating enough food per daySaturated Fat. On your Plate or in your BloodCufon.replace('p.Signature', { fontFamily: "komika" });#header p.tagline { color: #FFFFFF}.Signature […]
Drop this blog post from a cargo airplane in the form of flyers over Washington D.C.
I have never been able to penetrate their aerial defense system.
Question: You mention that coconut oil is a special case. Other sources I’ve read suggest that it is metabolized differently. Just as a matter of curiosity — does coconut oil function like any other fats in the matter of fat soluble nutrients?
Thanks.
I don’t know the answer to that. My guess is yes since it is still very hydrophobic, that is lipid-like.
Regarding a cholesterol count of 217, there is an analysis of diseases over many nations showing that the range of 200-250 cholesterol is associated with the lowest rates of various diseases.
this sort of thing may be inconclusive, but it is the very same type of inconclusive association that was used to pump up the cholesterol scare in the first place. The chart is here http://perfecthealthdiet.com/?p=3836
and there is a paper about the theoretical benefits of high LDL cholesterol here
“High cholesterol may protect against infections and atherosclerosis”
http://qjmed.oxfordjournals.org/content/96/12/927.long
If TG is low, then LDL will be mostly larger particles which are not associated with plaque formation.
There is “good” and “bad” LDL, “good” and “bad” lipoprotein, from the point of view of heart disease risk at least, but the tests to determine these are much more fiddly and expensive. So they’ll just keep looking for your keys under the lamppost, because that’s where all the light is.
Sometimes the light is out.
This calculator will give total cholesterol if you feed in the data on LDL, TG and HDL http://www.hughchou.org/calc/chol.php
that gives your total cholesterol as 381 or “very high”
However, according to the calculator all your ratios are “ideal”: in fact, some seem, if possible, better than that.
Your Total Cholesterol of 381 is HIGH RISK
Your LDL of 217 is VERY HIGH RISK
Your HDL of 157 is OPTIMAL
Your Triglyceride level of 39 is NORMAL
RATIOS:
Your Total Cholesterol/HDL ratio is: 2.43 – (preferably under 5.0, ideally under 3.5) IDEAL
Your HDL/LDL ratio is: 0.724 – (preferably over 0.3, ideally over 0.4) IDEAL
Your triglycerides/HDL ratio is: 0.248 – (preferably under 4, ideally under 2) IDEAL
Thanks. I have pointed this out to my doc. It is indeed confusing, perhaps even “paradoxical,” from the conventional point of view.
I think the elite lipidologists, such as Dayspring, would say to more or less forget about all of this and proceed to measure the lipoprotein particle counts. Nowadays, *that* seems to be what they think is actually causal for CVD.
This is probably in my future—not because I’m convinced the particle counts are any more interpretable than the earlier metrics, but because I hope the results will mollify my doc and bring us at least somewhat closer together on this.
There is also the next level. If a drug is recommended on the basis of a lipid parameter, how strong is the correlation between any proposed benefit of that drug and the lipid parameter?
“If a drug is recommended on the basis of a lipid parameter, how strong is the correlation between any proposed benefit of that drug and the lipid parameter?”
I have the feeling that this, plus simple observational correlation between, say, LDL-P and CVD, is what has led to the newer ideas about which measures really matter causally. I have not so far dived in to check this out.
I believe that “adverse events” under statin therapy don’t correlate terribly well with degree of cholesterol reduction, which of course leads to doubts about whether the cholesterol really matters. I’m guessing they correlate better with LDL-P, the new darling of the lipidologists. Which still does not convince me of causality, since the drugs are certainly pleiotropic and many things in biology track together.
Great post! We have very similar viewpoints, and I think you do an excellent job of conveying your information!
Very interesting post.
Some critics. Regarding Jakobsen study, why don’t you refer to the most comprehensive and recent meta-analysis on randomized outcome trials, ie. Hooper et al. 2011 (Cochrane systematic review)? You always call for exact and fair referencing – and hard end point RCTs are at the top of the evidence based hierarchy. The results do not change, though.
This all looks good for low carb diets in short term up until 6 and in some cases up until 12 months. Why aren’t you pursuing a long term outcome trial? These short term trials won’t be enough. Soon you you will find out how Mediterranean diet performs vs low fat AHA diet in really large scale trial, Predimed from Spain. When do get anything similar with a really low carb diet? Aren’t people purely unable to comply with the prescribed low carb diet in long term?
Thanks for your comments but I think you are discussing things that may have a number of assumptions that I don’t agree with. I am actually critical of the operation of the whole medical nutrition establishment.
Why don’t you refer to the most comprehensive and recent meta-analysis on randomized outcome trials, ie. Hooper et al. 2011 (Cochrane systematic review)? You always call for exact and fair referencing – and hard end point RCTs are at the top of the evidence based hierarchy. The results do not change, though.
Cochrane Systematic Reviews are self-appointed experts who I don’t recognize for any degree of understanding as in focussing only on RCTs which are good for some things, bad for others. On diet, they drastically increase error rate and are sustained at the top of the evidence-based library by medical researchers in a mindless way by virtue of their prestige (political power). In my view, RCTs have never recovered from Smith & Pell’s paper.
. The idea that one kind of experiment is appropriate for all questions is foolish and much like my Mozart story.
This all looks good for low carb diets in short term up until 6 and in some cases up until 12 months. Why aren’t you pursuing a long term outcome trial? These short term trials won’t be enough. Soon you you will find out how Mediterranean diet performs vs low fat AHA diet in really large scale trial, Predimed from Spain. When do get anything similar with a really low carb diet? Aren’t people purely unable to comply with the prescribed low carb diet in long term?
Who is “you.” I and others have applied for grants to do such studies but they will never be funded. The AHA, the NIH does not want to put these questions to the test. But do you need a long test? What is there about the low-carb diet, or more to the point, what is there the Volek-Westman principle, that is that the glucose-insulin axis is primary, what is there that makes you think that the effects won’t be sustained for as long as people stay on the diet? That medical researchers don’t want to separate adherence which, in any case, is better on low carb diets, with efficacy, only indicates the primacy of tradition over common sense in medicine. And the assumption of needing to prove the value of a low-carbohydrate diet assumes that there is an established dietary treatment for obesity diabetes and metabolic syndrome that is safe and effective. If we have that why are we still trying to do another low-fat, Mediterranean, low-GI, anything but low-carb trial? The value of low-carb is established. If you don’t like it do something else. But you may wind up like Lustig and Ludwig, frustrated and nasty, blaming the patient, recommending taxing, regulations and ultimately torturing the kid by taking him away from his parents. The sad part about resistance to funding, studying or even citing low-carb studies is that young investigators are afraid to look at the problem and many people are not offered the option. Low carbohydrate diets have better long term compliance than any other. If you think otherwise, show me the data.
I’ve been low carb since about 1968, and it’s been challenging at times, but not that much. That’s only n=1, but in that time I’ve seen more people stay on, and be successful at, a lower carb diet than a low fat diet.
In nutrition, anecdotal is important. We all see a lot of “patients” and we do three experiments a day so there are many n’s.
“Low carbohydrate diets have better long term compliance than any other.” Yes, in perhaps short term, ie. as long as the patients are willing to comply the restriction. I’m aware of the Adele Hite et al. paper.
There are three published trials that have lasted two years (Foster et al. 2010, Sacks et al 2009 ja Shai et al. 2008). In Foster et al. trial drop out was 42 % for low carb dieters and 32 % low fat arm.
In Sacks et al. 31/204 dropped during low fat phase, whereas 53/204 dropped out during low carb phase. In Shai et al.10/104 discontinued prematurely in low fat arm and 24/105 doscontinued early in low carb arm.
Drop out is circa two times higher among low carb dieters in long term trials. I haven’t got the access to Cerillo et al. 2009 which was the only 3 year trial. Anyway, that study has noxiously high drop out rates.
“what is there that makes you think that the effects won’t be sustained for as long as people stay on the diet?” Yes, this is the focal point of the problem. People have difficulties in resisting dietary variation (ie, having carbs like bread, pasta, potatoes, rice on the plate). If you restrict carbs, which are abundant in current western societies, you make the diet so much less palatable (acocording to many).
I appreciate the work you’ve done for patients and for science. Don’t get me wrong. Some research team will put together a long term trial on low carb diet, perhaps in Europe or Southern America. If receiving funding is very difficult, it doesn’t mean it’s impossible. Some party will fund it.
I assume that when you say “some party will fund it,” you mean that the Laatikainen family fortune will be used for the definitive diet study.
In any case, aren’t you making the intention-to-treat error that I discussed in another post? Whether you stay on a diet is largely separate from whether the diet works. If the diet is very effective but a Harvard professor tells you that you can’t stay on it, that can become a self-fulfilling prophecy. If the Harvard professor (Sacks) did not actually study any low-carbohydrate diets but only said that at a press conference, you have introduced a degree of uncertainty. Sacks study did not include a low-carbohydrate arm. Similarly, Foster said in public that he set out to trash the Atkins diet. That anybody in his study stayed on at all, is probably a miracle.
What these studies are is mindless addiction to a methodology that is scientism, what somebody told a doctor is how to do science. If you are interested in helping people, you would not sensibly focus on how hard the diet is. You would talk to people who have had success and ask why they stayed on the diet and you would use that information to help others stay on the diet. And remember, add up all the low-carb-low-fat comparisons and you have a few hundred people. The active low-carber forums is very close to 140,000 members and that’s just one internet group.
There are several questions on choosing a diet.
1) Is it based on sound science. Here you have to evaluate the biochemistry. I can help.I know some biochemistry. My guess is that whatever Frank Sacks knows about biochemistry, he learned from somebody like me, thirty years ago, but that doesn’t mean he is wrong. There are no real credentials in science. You have to evaluate it. It has a common sense side. It has a technical side and you can learn if you think diet is a critical part of health.
2) Is it safe? When you have an army of academic doctors, dietitians, whole health organizations trying to find something wrong with low-carb diets for forty years, and they can’t find it, it is probably the safest medical intervention known to man.
3) Does it work? Here you have to read the literature carefully, distinguishing between statements like “same at one year” when the data show that lipid markers were substantially better at one year. And, in diet, anecdotal evidence is good. People do three experiments a day for their whole life: everybody knows somebody who lost a lot of weight on the Atkins diet. Many never gained the weight back.
4) Finally, is it tolerable? I’ve been doing it for ten years and nobody has given me credit for general maturity or excellence of character. But, hell, you can try it. Given how safe it is, you can try it for a month. You can do anything for a month. And, instead of reading what Frank Sacks has to say about it, you can go on the internet and find out what people who have success think. They stay on it because they feel better and, as Tom Naughton says, they have a brain. They see that it is better for weight loss, glycemic control and atherogenic dyslipidemia. They can resist it, the way they resist alcohol. They don’t need some amateur social-planner to tax it. They can evaluate risks and rewards.
The real question is whether you care enough about diet to evaluate everything with an open mind. And, we are not pushing low carbohydrate diets, only fair access to the information and un-prejudiced options for the patient. We think that the science dictates that low-carb strategy of some kind is the “default” diet, the one to try first. If you don’t like it, you can try something else. But we could be wrong. Advantage for people who study low-carb is that we have a null hypothesis. Show us it is wrong and we will change our mind. I have no personal stake in this; I don’t own any pork-belly futures (whatever that is).
Maybe the dropout rate was higher in those studies, but out here in the real world, where people go low-carb because they *want* to, it’s said to be the easiest diet to stay on. Speaking only for myself, I’ve been low-carb for 3.5 years and very-low-carb (<10g/day) for over a year. Motivation needs to be taken into account.
The USDA and HSPH takes motivation into account when considering why their diets fail: if a low-fat diet fails it is the fault of the patient and their poor motivation. If a low-carb diet fails, it is the fault of the diet.
Reijo, my little two-cents’ worth here: The first point I was going to make has already been made above by Dr. Feinman. Many probably drop out of the low carb arm in these studies because they’re scared they’re ruining their health. My second point is my own experience with the variety issue. I’m not trying to do life-long Atkins induction. I’m somewhere between Barry Groves’s 50 grams and Lutz’s 72. Neither of those men had a list of forbidden foods. If I want to eat a bit of potato or rice or whatever, I do. I just keep my portions small enough to stay with my program. I never feel deprived. Looking back to my misguided low-fat years, I can tell you THAT’s deprivation, restriction, boredom, hunger . . . !
There you go again, giving us real data, real experience, instead of conjecture and “concerns.”
I guess “Feinman family fortune” has more potential 😉 Anyway, there are large interventions done in Europe as well. Often they get funded by some other party than AHA or NIH. Time will tell.
“Is it safe”, this is the tricky question. What do you think of all the prospective cohort data that exists and to large extend underlines the CV and cancer risks of low carb model (Lagiou et al, Trichopoulou et al., Fung et al. *2)? I know that low carb advocates have hard time accepting any cohort data opposing their views. But is these data worse han Jakobsen et al. ?
I have read the literature relatively well, or what do you think: http://slidesha.re/ybj9NP I’ve been following your publications, Volek’s and Krauss’ (even the last one on beef).
In any case, a long term trial would be very hard to ignore, even for those who you call for “Low Fat M****”. And finally, I think all the RCTs and meta-analyses on low carb diet have given fresh new air into the nutrition circles.
Dietitian RL from Finland
PS. Swedish dietary guidelines since November 2011, officially and bluntly recommend moderately low carb diet for type 2 diabetics (as one alternative). Ketogenic low carb diet is not recommended
“I know that low carb advocates have hard time accepting any cohort data opposing their views.” First, I am not an advocate for anything. I don’t have a hard time accepting data if it is good. I discussed what I think of these studies in other posts. However, how hard a time will you have if I suggest to you that all the prospective cohort data are not good, would probably not be admitted as evidence in a court of law in a toxic tort case and do not meet reasonable scientific standards? How hard is it for you to consider the possibility that these data show nothing — precisely because they are large and long period, they have tremendous variation and are usually designed with a hypothesis in mind that has little justification. How hard will it be for you to accept that? When they come up with an odds ratio of 1.5 and never, ever, show you the individual variation, you know that they have not shown you anything. Jakobsen does not show that SF is innocent. It shows (that is, all the accumulated studies show) that SF is not guilty. Like a court of law, you cannot be found innocent, only not guilty. Fat maybe bad, saturated fat may be bad and protein may destroy you kidneys but it has not been demonstrated and that’s what we know.
If you want to start from the idea that low-carb diets can be assumed guilty until proven innocent, you will have a hard time accepting contrary data.
A long term trial that was poorly done — the longer the trial, the less you have control over the relevant variables — then I will not have trouble ignoring it but, as in my post, I told George Bray how to do it right. The so-called “low-carb advocates” have to be in on the planning and analysis. Otherwise, it will be more inner circle self-congratulation. As for Swedish guidelines, recommendations are not data.
And “out here in the real world,” as TwitchyFirefly calls it, people are beginning to realize what is really good to eat and the price of meat, eggs and cheese is going up fast enough to really eat into the Feinman family fortune so we may still need the government…or the as yet undiscovered angel.
“Jakobsen does not show that SF is innocent. It shows (that is, all the accumulated studies show) that SF is not guilty. Like a court of law, you cannot be found innocent, only not guilty. Fat maybe bad, saturated fat may be bad and protein may destroy your kidneys but it has not been demonstrated and that’s what we know. ”
I could put it another way; what if saturated fat (whatever that means) and animal protein are in fact contributors to diseases BUT removing them from the diet or replacing them with ersatz or carbohydrate makes things worse? In other words we are all “born to die” and whatever we eat plays a role in this, and you can demonstrate this for any nutrient or food if you try hard enough, and there is only ever a “lesser evil” option?
Two reason for poor compliance on low-carb versus low-fat suggest themselves; there is a whole low-fat addictive junk health food industry to ensure compliance with low-fat, as well as carb craving (I hear heroin compliance is pretty good too). And, it’s more than likely that low-carb recipes in many trials are unappetising because there is still the idea that sat fat and red meat need to be limited for reasons that in any case should have nothing to do with the trial concept.
The trialer may be worried that if he doesn’t restrict the low-carb diet even further along politically correct food dogma lines his grant will be in danger.
On the second paragraph, you are asking the wrong question. Low-carb has much better compliance than low-fat. The table in Hite, et al. shows that in trials there is slightly better adherence. But as previously described, in the real world compliance is much better. Everybody knows this. The evidence is mostly anecdotal but that’s all there is on this question, low-fat or low-carb and anecdotally low-fat has terrible compliance. That’s why people are so fat given that the widely recommended diet is low-fat.
So, the important questions that we need to address
1. The people who have long term compliance to low-carb, why do they stay on the diet. What do they like about it and why do they think it is easy.
2. The other question is why people who can’t stay on low-fat diet, what their problem is.
Those are the questions. Any data on that?
“1. The people who have long term compliance to low-carb, why do they stay on the diet. What do they like about it and why do they think it is easy.”
I can offer one data point: After a few years of getting carbohydrate almost exclusively from non-starchy vegetables and some fruit, I have a hard time thinking of other sources as food, much less palatable food. I’ve tried adding grains, beans, or potatoes. Couldn’t do it.
Are you saying that your taste changed after being on a low-carbohydrate diet?
Yes, and it’s the most important reason that I find it easy to follow.
My study of one.. 4 1/2 years of high fat low carb, usually <20, always <50… real food "paleo" eating. Over 120 lbs gone, easy to maintain, vibrant health, great sleep, lots of energy, never hungry between meals, no cravings..
My low fat starvation diets of the past… I lost about 100 lbs 2 different times in my life via <1000 calories per day, nearly zero fat, small amounts of protein, mostly carbohydrate eating.
Always hungry, tired, constant cravings, an overall feeling of malaise… Each time, I stopped and went back to my regular high carb, high calorie, low fat diet when my hair started to fall out by the handful and, of course, regained all the pounds I had just lost.
Low carb works, and it's healthy… I am living proof.
In today’s post, I will describe the upcoming meeting in Washington, DC where I will moderate and speak at a session on “The Crisis in Nutrition.” One of the talks will be given by Tom Naughton (co-authors Jimmy Moore and Laura Dolson) called Vox Populi which will emphasize the importance of all the different studies of one.
Otago University researchers published a list of “needn’t” foods as a guide for the obese.
In it they recommended replacing butter, dripping and the like with oil and ersatz.
I wrote a letter to the editor in response and it was published in the NZ herald:
Dear Sir/Ma’am,
there are foods on the Otago University dieticians’ list of 49
“needn’t” foods which proper scientific
enquiry indicates are likely to be linked to a rise in obesity and
other diseases.
These are concentrated sources of sugars, refined
starches, and polyunsaturated vegetable oils. There are other foods,
some high in calories, which cannot be linked to obesity in the same
way.
Consumption of dairy fat and whole milk, for example, tends to be
associated with lower BMI than consumption of low fat milk or
vegetable spreads. The rise in obesity and related diseases has
followed in the wake of the low-fat diet fad and the rising use of
polyunsaturated vegetable oils.
The claim that an ancient food rich in protective nutrients is
responsible for a modern epidemic is an extraordinary claim, and
extraordinary proof needs to be supplied before any ancient food can
be lumped together with modern junk foods.
Criteria of calorie density and portion size, without taking into
account the differential metabolic effects of various nutrients, do
not meet an adequate scientific standard.
I agree on that low carb diets per se are often blaimed unfairly if participants don’t addhere to diet. I simply think that there are too much easily eaten carbohydrates available. Think if we wouldn’t only have all processed stuff like buns, sodas, snacks and sweets so easily available. It would be much easier to follow low carb diet.
Good questions. Who has got the answers? In addition, why people do not stay on high protein diet either (Krebs et al. 2012, Souza et al. 2012)? To what diet, people addhere ≥1 year in a randomized setting? Time to abandon randomization principle in long term dietary trials?
We are advised to change what we eat. There is plenty of everything around.
It is not the randomization principle that needs to be abandoned — that is useful — it is the implementation of the experiment and the uncritical acceptance of “statistical significance,” without asking whether it is meaningful, and the idea that longer times are necessarily better. If you have immediate good strong results and if there is no theoretical reason to think that there is risk then a long term study with poorly controlled variables that has an odds ratio of 1.5 is meaningless compared to the strong immediate effect. Short term positive effects with drugs have everybody excited until they are banned for “health concerns.” Short term positive effects with non-standard diet are viewed with suspicion and everybody tries to think of what is wrong.
“Short term positive effects with drugs have everybody excited until they are banned for “health concerns.” Short term positive effects with non-standard diet are viewed with suspicion and everybody tries to think of what is wrong.”
Spot on.
I completely agree with these viewpoints. I have personally lived on the low-fat high carb diet for almost 30 years and yet kept gaining weight and had a completely screwed up lipid profile. The Dr. almost put me on statins and thats when I decided to take matters in my own hands and started investigating exercise and good fats for heart health. I was of course shocked to not find a single piece of evidence that correlated dietary cholesterol to lipid cholesterol. I then started investigating saturated fats and still couldn’t find any evidence that saturated fat will cause heart attacks. I think when it comes to heart disease most of the medical community works off of hearsay where a doctor goes up on stage and announces, as-a-matter-of-factly, that cholesterol and saturated fats cause heart attacks and then the other doctors cite the previous doctor in their publications and so on and so forth. Its a vicious circle that’s been perpetuated for the last half a century and its time the medical community come clean. I highly doubt that’s ever going to happen given the fact that demonizing cholesterol has created a $26 billion industry of statin drugs that sponsors more research in this area. If you are a medical researcher serious about your career you better not say anything that will go against conventional wisdom of “cholesterol is evil” otherwise your grants will be cut and you will never publish any thing ever again. So from that standpoint I think the situation is abysmally bleak, but thanks to people like you there is some hope for people that are willing to take health matters in their own hands. Thanks for taking the initiative to educate the ordinary people about whats healthy and whats not!
Regards,
Yogesh Verma
inutrifit.com
I think things are not bleak and, in fact, have reached some kind of breaking point. At the upcoming conference produced by the Office of Research Integrity on March 14 and 15, I will chair and speak at a session on the “Crisis in Nutrition.” In the next few days, I will provide information about this and how we can try to exploit the opportunity to bring out the big issues and what can be done to correct them.
Thanks for explaining this so clearly. I appreciate it! 🙂
Bill, your lipids are actually very similar to mine except I have even higher LDL (so ratios are not ideal).
total Ch 8.9
fasting TG 1.3
HDL 1.65
LDL 6.7
(doesn’t quite add up I know, I took it over the phone, but right enough)
This was after deliberately excluding carbs and vegetable PUFA more than I usually do, just to see what would happen. Paul Jaminet has an explanation for this; in some people, extreme carb restriction induces a down-regulation of T3 thyroxine (by conversion of T4 to reverse T3) to conserve glucose and fat reserves. T3 also regulates LDL receptors, so a rise in LDL is one symptom, as well as some signs of hypothyroidism (but not all, as this change is adaptive, not pathological). Signs include sore or puffy eye sockets, loss of energy, loss of hair on outer eyebrows.
http://perfecthealthdiet.com/?p=4457
I think a lot of people don’t appreciate, not having actually read the books, that Dr Atkins never recommended being zero carb, or in full-blown ketosis, for longer than a fortnight. A great deal of Atkins diet counselling is around the re-introduction of carbohydrate, in limited, calibrated, amounts, in order to maintain the weight loss begun in ketosis.
I don’t think for a moment that this lipid profile reflected anything except the conditions that directly caused it. If you elevate LDL by eating huge amounts of sugar, this will probably be bad for your heart. If it comes about thru a nutritious paleo diet, that’s not quite the same thing at all.
The focus on the heart is a bit misleading too, given the different risk factors for cancer or suicide, deaths which involve considerably more suffering. Uffe Ravnskov used to ask those worried about heart failure, do you know of a better way to die?
” in some people, extreme carb restriction induces a down-regulation of T3 thyroxine (by conversion of T4 to reverse T3) to conserve glucose and fat reserves.” Is this from real data?
Thanks, George. My rT3 was recently measured and is “normal” (though I’m not sure anyone knows what that really means outside of overt illness). So even if Paul J’s theories on this are correct, it does not explain my LDL level.
I am hypothyroid, but it is carefully treated with supplemental T4 and T3 thyroid hormone. My total and free T3 are “low,” but again I’m not sure anyone can really say what that means in a healthy person. My endocrinologist, who probably has more experience using combined T3/T4 treatment for hypothyroidism than anyone else, has found T3 serum levels to be so uncorrelated with patients’ well being that he does not even measure them.
In terms of compliance and success on low-carb in the real world, my gf’s experience is instructive and, judging by the long-term studies, fairly typical. Gaining weight incrementally in late 30’s, esp after quitting smoking, she eventually tried Atkins last year. Lost about 14Kg in the first six months; and that was with frequent cheats or breaks. A longer break over Xmas saw her gain back 6Kg; going back on the diet this past two weeks has made no difference, whereas a loss of at least 1Kg would have been a reasonable expectation before.
However: she does not gain weight on the diet, even when it is interpreted liberally. And, she is by every possible indication healthier and fitter in every way than she was before. No longer snores, can swim a mile without stopping, and no longer exhausted after work, better moods, and so on.
So that, if for example she did want to take diet or exercise further, she would be ideally placed physically and psychologically to do so; if not, she has ample reason to be happy with where she has got to, and what she has achieved with so little in the way of inconvenience.
Dr Feinman, following the whole “safe starches” and LDL-rT3 controversy further, I find your name and views in the discussion, for example here: http://livinlavidalowcarb.com/blog/paul-jaminets-response-to-the-critics-of-his-safe-starches-concept/11920
Some points that ocur to me:
– If 100gm starch per day is still low-carb, which it obviously is, then there is no controversy, it is just allowing the proper range of variability under the low carb paradigm
– Many people who benefit from “safe starches” now, started by benefitting from ketosis (Kurt Harris, for example). I think in many cases the two are linked. A period of ketosis enables one to benefit from small amounts of starch later, but these might not have been so desirable before the ketosis period. I favour intermittent ketosis myself, and I find that the 100g safe starches really brings out the benefits of the ketogenic diet periods. But then I am not dealing with obesity, just recovering from metabolic imbalances.
– The rT3-LDL thing is natural and possibly life-prolonging. But personally, I don’t want some Struldbrugg form of longevity, I’m looking for ebullience, more abundant life here and now. That’s why calorie restriction doesn’t appeal to me.
– Ketosis is a medicine and sometimes we need to take our medicine.
– It is pretty obvious that most cereal grains and legumes are more toxic to the digestion than staple root and tuber starches. No shortage of research on this point.
– We are not Inuit, any more than we are Kitavans (pace any Inuit of Kitavans reading this). Inuit have prolonged epigentic adaptation to a zero-carb diet, and epigenetics may overall be more relevant than genetics in relation to glucose utilization.
[…] Kitavans, chers à Staffan Lindeberg. Que pensez-vous qu’il puisse arriver ? Hé bien, le taux d’acides gras saturés dans le sang augmente très fortement, sous forme de triglycérides, bien plus que dans le cas d’une alimentation riche en ces mêmes […]
I think Jaminet is looking for niche to sell some books. I find the use of term “safe starches” (compared to what Cake?) and the notion of a set needed level of carbohydrates consumption because a scare based on anecdotal evidence is very troublesome. I find this new fad on the blogosphere of disregarding the science to follow some guru opinion very disappointing.
Rawn Fulton of Searchlight Films, who will be working with Nutrition & Metabolism, pointed out that starch may not even be safe for your clothes and he pointed me to the story by S.J. Perelman entitled “No Starch in the Dhoti, S’il Vous Plait.”
According to Wikipedia, it began with “an off-hand phrase in a New York Times Magazine article (‘…the late Pandit Motilal Nehru—who sent his laundry to Paris—the young Jawaharlal’s British nurse etc. etc. …’), Perelman composed a series of imaginary letters that might have been exchanged in 1903 between an angry Pandit Nehru in India and a sly Parisian laundryman about the condition of his laundered underwear.
Personally, I think safe sex is better than safe starch.
Is it necessary to insist that a very low carbohydrate, ketogenic diet is always better than a low carbohydrate diet? Doesn’t the evidence rather support the view that both ketogenic (<50g carbs) and low carbohydrate diets (50-150g carbs) are superior to low fat or food pyramid diets?
I would point out that "the science" can only inform our thinking – science does not create diet plans, write recipe books, supervise our training regimes etc. There is a lot of science out there and no single study can confirm it all; no GP writes the same prescription for every patient.
(Well, maybe statins…)
Paul Jaminet is probably the most conscientious blog "guru" I've come across, Kurt Harris has no book to promote and doesn't offer advice, they have both done their homework. Both of them state clearly that ketogenic diets are desirable in a range of conditions, that carbohydrate becomes toxic as the level in the diet increases.
We were born to burn a little glucose along with the fat and ketones, so why shouldn't it be desirable at times to get some from our food?
I don’t insist on anything. In fact, diet is a catch-all phrase and applies to how you test the principles which I refer to as the Volek-Westman principle, that is, that the glucose-insulin axis is primary. What we know about the details is much less than what we don’t know. I think Volek and Westman agree with that. I teach medical students that the science points to a default diet for diabetes and metabolic syndrome, that is, the one to try first. If it doesn’t work well, or you don’t like it you can try something else. And, I point to the fact that, if 60 % of the population is overweight or obese, that means that, with all the high carb stimuli, all the low-fat propaganda, the continental breakfasts and all that, 40 % of the population is not obese or overweight and that is just as important a biological fact. Our argument with the lipophobes is that they claim to have all the answers and have been unwilling to confront their critics but I think that is changing. Both ASBP-NMS meeting and Ancestral Health Symposium will have dialogues with give-and-take panels, although that is only a first step towards what I think is the need for outside adjudication.
Jaminet is the one setting a needed carbohydrate requirement or your are going to get sick. If you think the take away message a lay person is going to get away from that is that LC is ok you are wrong. Why concern myself with a diet that can great more help problems, that what I have. At least does attacking LC from the saturated fat have some flimsy evidence; his is just creating concern and confusion with hearsay. Between him and Guyenet are creating the idea on the common folk with metabolic problems that there no need for carb restriction. That low carbs – insulin have no bearing on health or weight loss. That you can get sicker without carbs all you need is “natural” food.
The message that got across among the common folk that you see goes something like: I LIKE MY CARBS SO THEY MUST BE HEALTHY. I HAVE BEEN EATING HIGH CARB ALL ALONG AND NOW I HAVE PROVE THAT THIS IS HEALTHY. THAT SOME ISOLATED ISLANDERS EAT MANY CARBS AND I LIKE TO BELIEVE THEY ARE HEALTHY; SO CARBS ARE GOOD FOR ME TOO!
Sam, I agree. I’ve found this recent development in the blogosphere extremely disappointing. My impression is that there are a number of people posting now who started out with a good idea, or a good experience with their personal health, who didn’t have a long, strong back log of information from which to draw for a frequent blog. Perhaps that is why some are defensive, and others are so quick to abandon their original positions.
The whole thing is very disappointing but the blogosphere is less disappointing that the medical literature which is supposed to have gatekeepers (peer review) and I think we have to ask for change. I think the Office of Research Integrity meeting which I will describe in a post on Monday maybe a first step.
“. . .if 60 % of the population is overweight or obese, that means that, with all the high carb stimuli, all the low-fat propaganda, the continental breakfasts and all that, 40 % of the population is not obese or overweight . . .”
Probably not possible, but it certainly would be interesting to find out whether there are any differences between the two groups — age, gender, genetic factors, actual diets, etc. — in spite of the fact that all are subject to the same high carb stimuli, low-fat propaganda, and such.
The real tragedy in the nutrition mess is that we are wasting so much money and effort on meaningless stuff that we can’t do the real research that needs to be done.
“The real tragedy. . . ” Or when they do get unexpected meaningful stuff from a study — I’m thinking of the WHI, in which low fat flunked in just about every area — they will spend the next 20 years saying it really isn’t so.
The WHI was supposed to do that. It FOLLOWED more than 20 years, maybe 40 years of unexpected meaningful stuff: when you are talking about changing your lifestyle, failure to show an effect is a big deal. Framingham, Techumseh, Bogulusa, Oslo, MR FIT…(would make an amusing song along the lines of Van Lingle Mungo ballad based on the names of baseball players, or Tom Lehrer’s Periodic Table.
I have a favor to ask of all you experts out there. I have informed the head of the health ministries at my home church that a “health tip” she had printed in the church newsletter saying that colon cancer is linked to diets high in animal fat and low in fiber was inaccurate and not scientifically supported. I sent one link to an article stating that saturated fat consumption was not in any connected to colon cancer, but she is asking me for more information. Can you supply links to studies (good, scientific studies) that debunk the high animal fat/low fiber theory of “cause” for colon cancer?
Thanks.
I think that if you want convincing analysis you are asking for something equivalent to sitting in judgement on a law case which involves some time and research and, in essence, involves evaluating evidence as if in a court of law.
I am prepared to take on this case but it will help to know if the head of the health ministries wants such an analysis or have you already “agreed to disagree.” Also, it is also important to understand that the judgement will rest on detailed analysis and scientific method. Clearly, red meat and low fiber in colon cancer are not like cigarette smoke in lung cancer. If it were, we would all know it and we wouldn’t be doing yet another epidemiologic study. So, it should be understood that the outcome as to whether there is a risk will probably address how big that risk is rather than yes or no. A big barrier may be the grounds for acceptance. Again, by analogy with legal proceedings, some states adhere to the so-called Frye standard which means “general acceptance” by the scientific community and, in practice may mean renowned authorities. So, interested parties have to consider that, for example, the Harvard School of Public Health may be wrong, way wrong in their methodology and interpretation despite their prestige. Conversely, you have to be prepared for the possibility that there really is a risk. In the absence of known mechanisms, one is inclined to put the burden of proof on the “plaintiff” but it may turn out that risk exists. (You can always appeal).
With those conditions, I will take your case and, of course, will ask all the other experts out there, to testify.
Fantastic post! very informative. I’ve been on a low carb diet for a almost a year and doing great other a persistent headaches of late which think might be related to macronutriant ratio so my question is….what macronutriant ratio would you advice as ideal to achieve the Volek-Westman principle? what carbohydrate level would tend to make fat consumption more dangerous
The point that I was trying to make is that principles are more important than particular diets where it is impossible to get any agreement on definitions and where individual variations in people and what they are trying to do becomes critical. The Volek-Westman principle says that carbohydrate, directly or indirectly through insulin and other hormones, controls what happens to ingested (or stored) fatty acids and therefore “a high fat diet in the presence of carbohydrate is different than a high fat diet in the presence of low carbohydrate.”
So, you don’t say what your goals, medical condition or current eating habits are or your and I would, in any case, not want to give you any specific advice. The principle says that carbohydrate is key. So if you have diabetes or metabolic syndrome you should probably eat as little carbohydrate as you are comfortable with — you have to work this out with your doctor — if you are on medication, it is a must since the diet may do the same thing that the drug does. If you are trying to lose weight the ratio of any fat to carbohydrate and the total intake is, obviously, the number that works.
The real-take home message is not to be afraid of saturated fats. It is possible, strange as it might seem, that we actually evolved with a sense of taste to give us a rough start on what’s healthy: I find 1:1 Olive oil (good quality but not virgin):butter is the best thing for frying an omelet.
V-W priniciple is primarily therapeutic and it’s application depends on the severity of the problem you are trying to deal with. If you are trying to feel good and get productive exercise, you have to find what works. Your headaches are unlikely to be due to the ratio of SFA to carbohydrate but you can experiment. You might want to reduce stress — have you been listening to Dr. Sanjay Gupta or other TV-doctors?
On the other end, if you are a serious athlete and want to explore the potential of ketogenic diets, you should get Volek and Phinney’s new Book on low carbohydrate “…Performance.” Actually, you should get it anyway. It is somehow a great introduction to the area. Since they are colleagues, I expected it was authoritative — the earlier “The Art and Science of Low Carbohydrate Living” is the best comprehensive introduction and naturally I would endorse it, but, maybe because the emphasis is on performance which I know less about, it really grabbed me. The book gives a real feeling for the principle.
I am sorry I can’t answer your specific question to which you will have to find your own implementation of the principle. If you want an absolute, authoritative answer with an exact number, you may have to call Dr. Gupta, Dr. Lustig or other TV-doctors. They’ve got it all worked out. I’m just a chemist.
[…] […]
I am a little perplexed by some studies being discussed at http://humanfoodproject.com/palm-oil-maybe-not-such-a-good-idea-after-all regarding effects of high fat diet. Here is a quote: “I have discussed elsewhere (here and here) the potential impact of a high-fat diet and changes in your gut microbial ecosystem that can (does) lead to low-grade inflammation that furthers leads to insulin resistance, obesity and other issues. In short, high-fat intake shifts the gut microbiota and increases the translocation of lipopolysaccharides (LPS) or endotoxins from your gut into your blood, which then triggers inflammation – and then the cascade of problems start.”
The studies cited are referenced at:
http://humanfoodproject.com/can-a-high-fat-paleo-diet-cause-obesity-and-diabetes/
http://www.ncbi.nlm.nih.gov/pubmed/22094473
I am not trying to set one person against another, but I am wondering if you were aware of these studies in rodents and if they do in fact have something to say about the human condition. If a high fat diet can have these effects, its of obvious concern to Paleo adherents.
With regard to the abstract, the response of C57Bl6 mice to fat is as likely to tell us about the opposite of what happens in humans as about anything else.
General comment is that this is not about hadron decay. It is about something we all have experience with. Low fat-high carbohydrate diets make my gut feel worse. How about you? And, at least anecdotally, people cure irritable bowel syndrome rapidly by reducing carbohydrate and going on a “high fat diet” which may only be fat in comparison to the uptight puritan diet recommended by non-scientists. And when you ask a gastroenerologist about low-carb diets curing IBS they will attribute it to change in gut microbiota.
“Low fat-high carbohydrate diets make my gut feel worse. . .” You and a lot of the rest of us.
“. . .a “high fat diet” which may only be fat in comparison to the uptight puritan diet recommended by non-scientists.” As long as these non-scientists persist in using % of total calories, a diet that is unchanged except for a significant reduction in carbohydrates, can suddenly end up a “high fat” diet.
[…] “when the blood of volunteers was assayed for saturated fatty acids, those who had been on a low carbohydrate diet had lower levels than those on an isocaloric low-fat diet. This, despite the fact that the low-carbohydrate diet had three times the amount of saturated fat as the low-fat diet.” Saturated fat. In your plate or in your blood? […]
Revisiting this post after 5 years, I find myself with one pressing question about the Volek-Westman principle – why myristic acid? It is C14:0 that is dropping significantly in a dose-dependent way with CHO restriction in all the papers on this subject, even as more is eaten, much more so than C16:0.
Of all the fats in the analysis, C14:0 also produces the largest rise in HDL in feeding studies (done with relatively low fat context). Carbohydrate restriction also produces a rise in HDL; so how is this all connected?
High C14:0 in serum is a marker for some diseases, notably NASH, https://www.ncbi.nlm.nih.gov/pubmed/21516322/
and is associated with low HDL, with a decent causal mechanism.
Noto, D et al. Myristic acid is associated to low plasma HDL cholesterol levels in a Mediterranean population and increases HDL catabolism by enhancing HDL particles trapping to cell surface proteoglycans in a liver hepatoma cell model. Atherosclerosis. 2016; 246:50 – 56